2. Department of Pediatrics and Community Health Sciences, University of Calgary;
3. Maternal and Infant Care Research Centre, Mount Sinai Hospital, University of Toronto, Canada
Neonates in the neonatal intensive care units (NICUs),especially those born very preterm,are one of the most vulnerable populations with high risk of developing serious complications,such as intracranial hemorrhage (IVH),bronchopulmonary dysplasia (BPD),infections and even death. Infection is the one of the most common morbidities in neonates admitted to the modern NICUs. Infection could be early or late based on the onset of sepsis. Early onset of sepsis occurring less than two days after birth,or late secondary onset sepsis,which typically occurs after two days of life and is considered nosocomial in origin. Nosocomial sepsis rates can vary greatly between hospitals,regions and countries[1, 2, 3]. Despite continued efforts,the nosocomial infection (NI) rates in NICUs in Canada remain extremely variable between units[4, 5]. The impact of this variability on neonatal outcomes has not been evaluated. Previous studies have shown that NI is associated with higher neonatal mortality and morbidity. Rates of NI increases with decreasing birth weight and gestational age,and often relate directly to the actions of health care workers[3, 6, 7],which can produce large variability in NI trends among hospitals. The cost of NI and associated morbidities is very high for institutions[8] with serious long-term effects on infants' health,such as learning difficulties,cerebral palsy,hearing impairment and visual impairment[9].
Coagulase-negative staphylococci (CoNS) are the most common pathogens implicated in late-onset sepsis[10]. Staphylococcus epidermidis is the primary species of CoNS associated with late-onset sepsis in both adult and pediatric patients[11, 12, 13, 14]. Methicillin resistant Staphylococcus capitis is emerging as a potentially significant pathogen in NICUs,causing late onset of sepsis in very low birth weight infants (VLBW) infants[14]. This pathogen is rarely found in adult patients[15] and strains in France have been found to show reduced vancomycin susceptibility[10]. Other common pathogens responsible for NI in NICUs include Staphylococcus aureus,gram-negative organisms,and candida infections[16].
About half of NICU-acquired infections manifest as bloodstream infections but they can also appear as lower respiratory tract,ear-nose-throat and urinary tract infections[17]. Complications of prematurity,which can lead to increased rates of NI,include patent ductus arteriosus (PDA),prolonged ventilation,prolonged intravascular access,BPD and necrotizing enterocolitis (NEC)[16]. Interventions associated with increased risk of bloodstream infections include central intravascular catheters and receiving total parenteral nutrition (TPN)[17].
Numerous interventions,including more stringent and sterile protocols for placing and maintaining indwelling venous catheters,have been implemented to decrease NI rates associated with medical care and procedures within NICUs in Canada through the Evidence-based Practice for Improving Quality (EPIQ) through CIHR research projects. Implementation of evidence-based guidelines for the prevention of hospital-acquired infections has resulted in reduced overall NI rates in Canadian NICUs from 2003-2009 [18]. Although the overall NI rate has decreased,Canadian Neonatal Network (CNN) data reveal significant variations in NI trend among Canadian NICUs. Further research is warranted to characterize these trends in NI rates,gain new knowledge about factors contributing to NI,and further delineate the associations of NI to mortality/ morbidities in Canadian NICUs.
While surveillance of NI trends in ICUs has been documented for adults,this information cannot be extrapolated to neonates [17, 19, 20]. The objective of this study was to characterize recent trends of NI among preterm infants admitted to Canadian Level 3 NICUs during 2008-2012,and its association with neonatal outcomes.
Materials and methodsThis observational study examined data from very preterm infants born with gestational age (GA) <33 weeks and admitted to NICUs affiliated to the CNN during 2008 to 2012. At all CNN participating sites,patient information was extracted by trained personnel using standard definitions according to the CNN Data Abstractor Manual. Information was entered into the database and was electronically pooled,stored and checked periodically for accuracy at the CNN Coordinating Center.
For this study,an admission was defined as a stay of >24 hours or death/transfer to another facility within 24 hours. Infants were excluded if born with major congenital anomalies,declared moribund (a decision was made at birth not to provide resuscitative care). We further excluded infants from NICUs with less than 15 infants admitted during any year during the study period.
Early onset of sepsis was defined as when sepsis occurring less than two days after birth,or late secondary onset sepsis,which typically occurs after two days of life and is considered nosocomial in origin.
A composite outcome was defined to indicate mortality (all causes during NICU stay) or any severe neonatal morbidity (intraventricular hemorrhage grades 3-4 or periventricular leukomalacia,retinopathy of prematurity stages 3-5,bronchopulmonary dysplasia or necrotizing enterocolitis stages 2-3).
Statistical analysesNICU sites were classified into three groups with equal number of sites according to baseline NI rates during 2008: Low (≤14%),Medium (14.1%- 19%) or High (>19%) NI groups. The pattern of NI rates was evaluated within each NICU site using the Cochrane-Armitage trend test,and NICU sites were also classified according to their NI trend: decreased [Cochrane-Armitage test P≤0.2],null [P>0.2] or increased [P≤0.2]. Since the number of infants with GA <33 weeks admitted to each site for each year may be too small to be able to detect the trend at the significance level of 0.05,therefore we used 0.2 as the cut-off to group the sites with similar pattern of NI rate. Infant characteristics and treatment procedures were summarized across baseline-NI and trend-NI groups and tested for association using the Pearson Chi-square test and the ANOVA F-test for categorical variables and continuous measures,respectively.
For each of the three baseline-NI groups [Low group (≤14%),Medium (14.1%-19%) and High group (>19% %)] and NI trends (decreased,null and increased),NI rates were evaluated using multivariable logistic regression with adjustment for potential confounders and important risk factors. Trends in the composite outcome and each of its components were tested within each trend-NI group separately using multivariable logistic regression analyses. All statistical analyses were performed using the SAS software,version 9.3 (SAS Institute Inc. Cary,NC),with statistical significance evaluated using 2-sided P values at the 5% testing level.
ResultsThere were a total of 18 961 infants that met the inclusion criteria from 24 NICU sites participating in the CNN. Table 1 and Figure 1 reports yearly NI rates of each NICU site during the study period,and indicates the classification of each site according to baseline-NI rate in 2008 and trend-NI during the study period. Tables 2 and 3 show the distribution of infant characteristics and treatments among NICU site groups defined according to baseline-NI rate and the trend-NI,respectively.
| Table 1 NI rates and trends for each participating NICU [%(n/N)] |
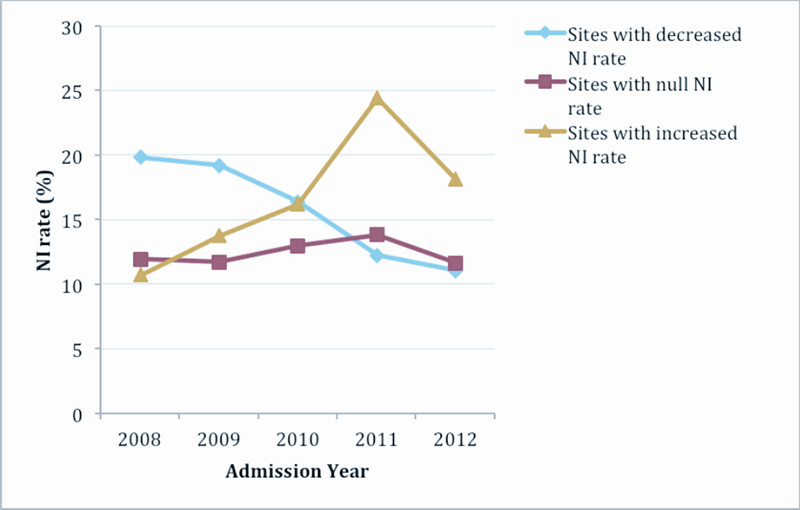 |
Figure 1 Trends of NI rates for three NI site groups This figure shows the trends for each of the three NI site groups: sites with decreased NI rate (P<0.001), sites with null NI rate (P=0.58) and sites with increased NI rate (P<0.001). |
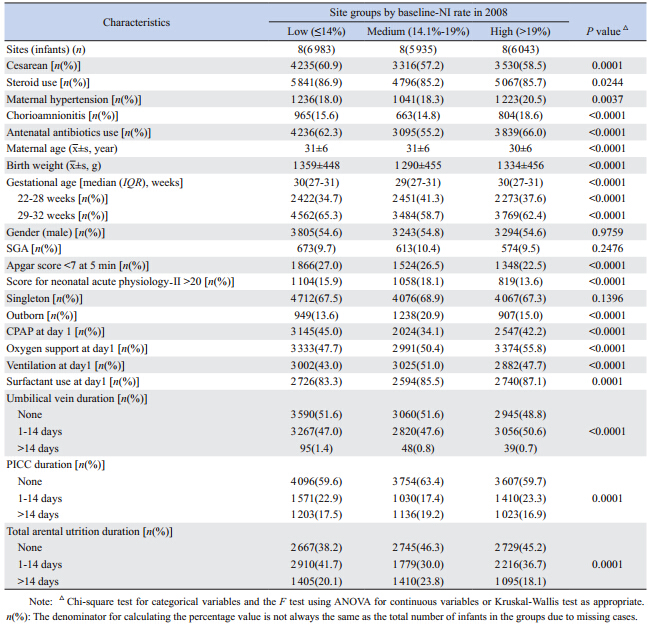
Interestingly gender,small for gestational age (SGA) or singleton status has no impact on the baseline NI rates in NICUs (Table 2). However,preterm infants born to younger mothers or mothers with hypertension or with chorioamnionitis or infants who needed oxygen or surfactant on day one of life or required umbilical venous or peripherally inserted central catheter (PICC) line were more likely to have high risk of baseline NI in NICUs (Table 2).
| Table 2 Distribution of characteristics among baseline-NI rate site groups |
The other factors like cesarean-section,premature infants (22-28 weeks),low birth weight,SGA,outborn,Apgar score <7 at 5 minutes,singleton and PICC line duration >14 days had increased trend of NI (Table 3). In contrast,babies born to younger mothers,receipt of antenatal corticosteroids or antibiotics,shorter duration of TPN,need of oxygen or use of CPAP on day one of life had decreased trend of NI in various NICUs (Table 3). However,there was no effect of maternal hypertension,duration of umbilical venous lines or PICC line catheters or use of surfactant on day one or gender on trend of NI in NICUs affiliated with the CNN (Table 3).
| Table 3 Characteristics among NI-trend groups |
For sites with high baseline NI rates,the trend in NI during subsequent years was decreased; however no significant NI trends were detected for sites with low or medium baseline NI rates (Figure 2).
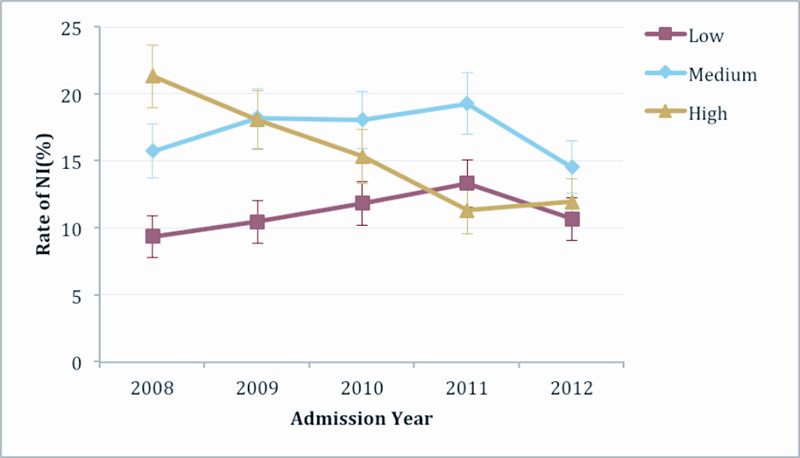 |
Figure 2 Trends of NI rates within site groups
classified according to baseline-NI rate NI rate decreased over time for High baseline-NI rate site group (P<0.0001); NI rate increased over time for Low baseline-NI rate site group (P=0.045); No increased or decreased in NI rate over time for Medium baseline NI rate group. After adjustment for gestational age, gender, small (<10th percentile birth weight) for gestational age, Apgar score < 7 at 5 min, score for neonatal acute physiology-II, singleton, outborn status, cesarean delivery, maternal hypertension, antenatal steroid use, maternal antibiotic use and maternal age, only the trend in NI rate for High baseline-NI rate site group remained (adjusted OR: 1.02 (0.96, 1.09), 0.94 (0.89,1.00) and 0.79 (0.74, 0.84) for Low, Medium and High baseline-NI rate site groups respectively). |
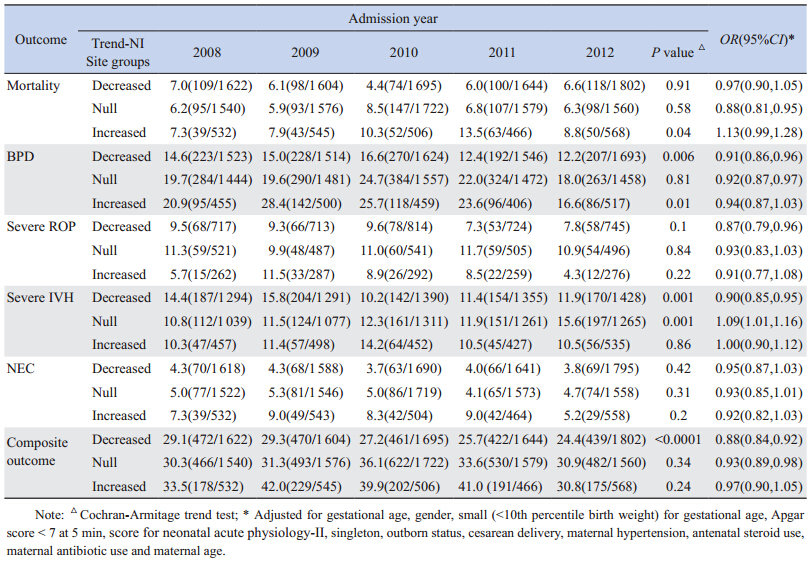
Table 4 shows the trends in the adverse neonatal outcomes within each of the three site groups classified according to the trend in NI rate. For example,the trend in the composite mortality/morbidity and BPD significantly decreased for sites with decreased NI trend (OR of composite outcomes=0.88,95% CI=0.84-0.92) or null NI trend (OR of composite outcomes=0.93,95%CI=0.89-0.98). No significant trend in the composite outcome was detected for sites with increased NI rates (Table 4). Similarly,the trend in severe retinopathy of prematurity (ROP) and severe IVH (IVH grade 3) also decreased significantly for sites with decreased NI rate (Table 4).
| Table 4 Trends in mortality, morbidities and the composite outcome within sites classified according to the trend in NI rates [%(n/N)] |
It remains important to quantify the relative contribution of NI and other neonatal care practices to mortality/morbidity to identify target interventions that will provide the greatest improvement in outcomes of preterm infants. The effect of NI baseline rates and NI trend on the short term and long term outcome is not well studied and recognized. As we strive to improve outcomes in the vulnerable population in NICUs,we need all the tools necessary in our hands to affect change and improve quality of life in this population.
NI is common among preterm infants admitted to NICU. In fact up to 50% of preterm infants < 26 weeks get NI during their stay in NICU [16]. Klinger et al [21] showed that VLBW infants with sepsis were at increased risk of BPD [OR: 1.74 (95%CI: 1.24- 2.43)],severe intraventricular hemorrhage (IVH) [OR: 2.24 (95%CI: 1.67-3.00)],and severe ROP [OR: 2.04 (95%CI: 1.32-3.16)]. The increased risk of IVH,BPD and ROP in infants with sepsis is associated with a direct bacterial effect by cytokine-mediated inflammatory response,increased exposure of infants with sepsis to mechanical ventilation and exposure to prolonged oxygen therapy. In this study based on national database,we found that the rates of BPD,severe ROP,and IVH grade3 were all significantly decreased in sites with decreasing NI rate possibly due to reduced inflammatory response.
Overall mortality in this group was not changed significantly. This study revealed improved outcomes in sites with null trend in NI,the composite outcome showed greater change in the sites with decreased NI rates. This correlation provides us with evidence that our efforts to decrease NI rates is contributing to improved quality of life in neonates due to lower rates of major morbidities. We found decreased rates of mortality and major morbidities also in sites with null trend in NI. This is likely due to improved techniques and treatments in NICUs unrelated to NI rates. No decrease or increase trend for mortality and morbidity was observed in the site group with increased NI rate. The sites with low baseline NI rate may not target to improve their NI rate but may conduct the interventions targeting to improve other morbidities. Instead,the sites with high baseline NI rates may conduct interventions to decrease the rate. This may explain why NI rate decreased for those sites with high baseline NI rate. This also may have been mitigated by the same improvements in treatment and techniques leading to improved outcomes in the group with no changes in NICU rate.
When subdivided by baseline NI rate,we found that the trend of NI rate was impacted significantly. For example,in the low baseline NI rate group,NI rate increased significantly (although not significant when adjusted),while in high baseline NI rate group,NI rate decreased significantly,even after adjustment. No increase or decreased trend was observed for the average baseline NI rate group. We believe that these trends are partly a result of large scale interventions aimed at decreasing the NI rates. These interventions had the greatest impact on hospitals with high baseline NI rates and brought them closer to the rates of other hospitals,which were likely already,implementing stringent infection control protocols.
In conclusion,the neonatal outcome is influenced by NI rates and trend. The trend in the composite mortality and the risk of BPD,severe ROP and IVH were significantly decreased for site group with decreased NI rate. These decreased outcomes were associated with effort to decrease NI rate and may also lead to a decrease in other adverse neonatal outcomes.
Based on our findings,these efforts have led to improvements in sites with previously higher than average NI rates. Therefore,we must continue to monitor NI rates in nurseries and continue to strive to maintain low rates of NI in order to improve quality of life in this vulnerable population. Future studies of NICU outcomes should take this into account in planning,data gathering and doing statistical calculations.
| [1] | Carrieri MP, Stolfi I, Moro ML, et al. Intercenter variability and time of onset:two crucial issues in the analysis of risk factors for nosocomial sepsis[J]. Pediatr Infect Dis J, 2003, 22(7):599-609. |
| [2] | Moore DL. Nosocomial infections in newborn nurseries and neonatal intensive care units [M]//Hospital epidemiology and infection control. Williams & Wilkins, Baltimore;1996:535-564. |
| [3] | Kawagoe JY, Segre CAM, Pereira CR, et al. Risk factors for nosocomial infections in critically ill newborn:a 5-year prospective cohort study[J]. Am J Infect Control, 2001, 29(2):109-114. |
| [4] | Lee SK, McMillan D, Ohlsson A, et al. Variations in practice and outcomes of the Canadian NICU Network:1996-7[J]. Pediatrics, 2000, 106(5):1070-1079. |
| [5] | Chien LY, Macnab Y, Aziz K, et al. Variations in central venous catheter-related infection risks among Canadian neonatal intensive care units[J]. Pediatr Infect Dis J, 2002, 21(6):505-511. |
| [6] | Sohn AH, Garrett DO, Sinkowitz-Cochran RL, et al. Prevalence of nosocomial infections in neonatal intensive care unit patients:results from the first national point-prevalence survey[J]. J Pediatr, 2001, 139(6):821-827. |
| [7] | Nagata E, Brito AS, Matsuo TL. Nosocomial infections in a neonatal intensive care unit:incidence and risk factors[J]. Am J Infect Control, 2002, 30(1):26-31. |
| [8] | Johnson TJ, Patel AL, Jegier BJ, et al. Cost of morbidities in very low birth weight infants[J]. J Pediatr, 2013, 162 (2):243-249. |
| [9] | Mwaniki MK, Atieno M, Lawn JE, et al. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults:a systematic review[J]. Lancet, 2012, 379(9814):445-452. |
| [10] | Rasigade JP, Raulin O, Picaud JC, et al. Methicillin-resistant Staphylococcus capitis with reduced vancomycin susceptibility causes late-onset sepsis in intensive care neonates[J]. PLoS One, 2012, 7(2):e31548. |
| [11] | Kirchhoff LV, Sheagren JN. Epidemiology and clinical significance of blood cultures positive for coagulase-negative Staphylococcus[J]. Infect Control, 1985, 6(12):479-486. |
| [12] | Kim SD, McDonald LC, Jarvis WR, et al. Determining the significance of coagulase-negative staphylococci isolated from blood cultures at a community hospital:a role for species and strain identification[J]. Infect Control Hosp Epidemiol, 2000, 21(3):213-217. |
| [13] | Herwaldt LA, Geiss M, Kao C, et al. The positive predictive value of isolating coagulase-negative staphylococci from blood cultures[J]. Clin Infect Dis, 1996, 22(1):14-20. |
| [14] | Klingenberg C, Ronnestad A, Anderson AS, et al. Persistent strains of coagulase-negative staphylococci in a neonatal intensive care unit:virulence factors and invasiveness[J]. Clin Microbiol Infect, 2007, 13(11):1100-1111. |
| [15] | Ruhe J, Menon A, Mushatt D, et al. Non-epidermidis coagulasenegative staphylococcal bacteremia:clinical predictors of true bacteremia[J]. Eur J Clin Microbiol Infect Dis, 2004, 23(6):495-498. |
| [16] | Stoll B, Hansen N, Fanaroff A, et al. Late-onset sepsis in very low birth weight neonates:the experience of the NICHD Neonatal Research Network[J]. Pediatrics, 2002, 110(2 Pt 1):285-291. |
| [17] | Sohn A, Garrett D, Sinkowitz-Cochran R, et al. Prevalence of nosocomial infections in neonatal intensive care unit patients:results from the first national point-prevalence survey[J]. J Pediatr, 2001, 139(6):821-827. |
| [18] | Shah PS, Yoon W, Kalapesi Z, et al. Seasonal variations in healthcare-associated infection in neonates in Canada[J]. Arch Dis Child Fetal Neonatal, 2013, 98(1):65-69. |
| [19] | Welliver RC, McLaughlin S. Unique epidemiology of nosocomial infections in a children's hospital[J]. Am J Dis Child, 1984, 138(2):131-135. |
| [20] | Harris JA. Pediatric nosocomial infections:children are not little adults[J]. Infect Control Hosp Epidemiol, 1997, 18(11):739-742. |
| [21] | Klinger G, Levy I, Sirota L, et al. Outcome of early-onset sepsis in a national cohort of very low birth weight infants[J]. Pediatrics, 2010, 125(4):e736-e740. |
 2015, Vol. 17
2015, Vol. 17