川崎病(Kawasaki disease, KD)是以全身性血管炎为主要特征的发热性疾病,全身性炎症反应在川崎病的发病机理中起重要作用[1]。未控制的持续性炎症可导致不良后果如冠状动脉扩张和静注免疫球蛋白(intravenous immune gobulin, IVIG)不敏感,炎症性生物标志物可能有利于川崎病的诊断及预后判断[2]。但川崎病到目前为止尚缺乏特异性的生物学标志物,其诊断主要依靠临床表现,实验室检查仅作为支持手段[3]。白细胞是重要的炎症介质,白细胞计数及其亚群分类是经典的炎症指标,当全身性炎症刺激免疫系统时血白细胞数量将发生改变,一般认为中性粒细胞是非特异性的炎症标志物,而淋巴细胞是免疫调节反应的标志物,因此中性粒细胞与淋巴细胞比值(neutrophil-to-lymphocyte ratio, NLR)是炎症反应和免疫平衡的反映[4-5]。有研究报道,NLR是手术应激、全身炎症反应、脓毒症的有效标志物,疾病严重程度与中性粒细胞增多及淋巴细胞减少有关[6]。还有研究显示,NLR以及血小板与淋巴细胞比值(platelet-to-lymphocyte ratio, PLR)均是十分重要的系统性炎症标志物和心血管不良事件预测指标,联合应用NLR和PLR有助于预测心血管事件发生和经皮冠状动脉介入治疗的风险[7-9],还可预测恶性疾病的不良预后[10]。川崎病急性发热期白细胞的增高以中性粒细胞增高为主,国外有研究显示联合应用NLR和PLR可以预测川崎病患者冠状动脉病变发生[11-13],但是关于NLR和PLR与川崎病IVIG敏感性关系的报道较少。本文采用回顾性队列研究的方法,分析NLR和PLR对于预测川崎病患者IVIG敏感性的价值。
1 资料与方法 1.1 研究对象选择我院2000年至2016年收治的404例初诊KD患者为研究对象,其中IVIG敏感者373例,IVIG不敏感者31例。所有患者均符合川崎病的诊断标准[14]。本研究病程第1天定义为发热第1天。IVIG不敏感定义为首次IVIG治疗36 h后体温仍超过38℃或热退2~7 d后再现发热,并伴有至少一项川崎病的主要临床特征[15]。冠状动脉扩张的标准为: < 5岁,冠状动脉内径 > 3 mm;≥5岁,冠状动脉内径 > 4 mm;冠状动脉瘤诊断标准为冠状动脉局限性或弥漫性扩张,其直径超过相应年龄正常值1.5倍,内径4.1~4.9 mm的为小冠状动脉瘤,5.0~7.9 mm为中等冠状动脉瘤,≥8 mm的为巨大冠状动脉瘤[16]。
1.2 治疗方法所有患者急性期均口服阿司匹林(每日30 mg/kg)、静脉使用IVIG(每日1 g/kg×2 d)。分析IVIG治疗前后的血常规,NLR和PLR。血常规采集时间点为IVIG使用前的急性发热期、IVIG结束后第2天。心脏彩超检查时间为入院时和IVIG使用后第2天,若无冠状动脉扩张,每2周检查1次心脏彩超,直至出院;若出现冠状动脉动脉扩张则每周检查1次直至出院。
1.3 统计学分析用SPSS 20.0统计软件进行数据处理。计量资料以均数±标准差(x± s)表示,组间比较采用方差分析或者t检验。计数资料用百分率表示,组间比较采用χ2检验。危险因素分析采用多因素logistic回归分析;ROC曲线确定NLR和PLR的最佳预测值。P < 0.05为差异有统计学意义。
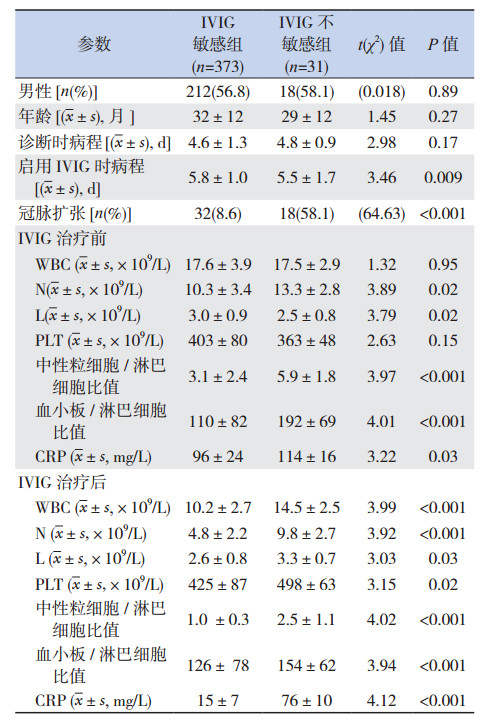
2 结果 2.1 IVIG敏感组和不敏感组的临床资料分析404名患者纳入该研究,31名(7.8%)对首次IVIG不敏感。与IVIG敏感组相比,IVIG不敏感组的冠状动脉扩张发生率明显增高(P < 0.01);启用IVIG时的病程较短(P < 0.05);IVIG治疗前后的NLR、PLR水平以及CRP均较高(P < 0.05)。治疗前两组白细胞总数的差异没有统计学意义(P > 0.05),但是IVIG不敏感组的中性粒细胞数较高(P=0.02),淋巴细胞数较低(P=0.02)。见表 1。
| 表 1 川崎病IVIG敏感组和IVIG不敏感组的临床资料比较 |
2.2 IVIG治疗前后NLR、PLR对于川崎病IVIG敏感性的预测价值
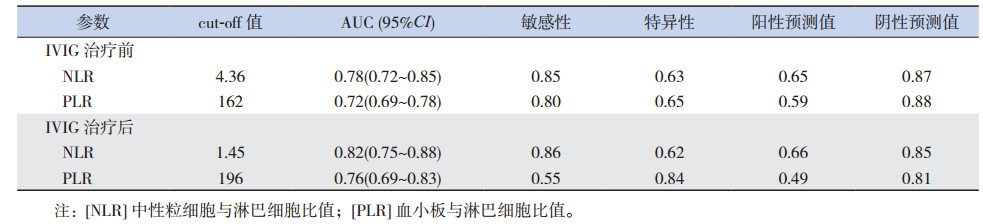
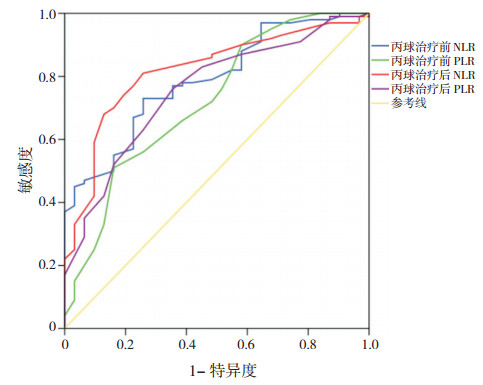
IVIG治疗前NLR和PLR预测IVIG不敏感的最佳cut-off值分别是4.36和162,曲线下面积分别是0.78和0.72(95%CI:0.72~0.85和0.69~0.78);IVIG治疗后NLR和PLR预测IVIG不敏感的最佳cut-off值分别是1.45和196,曲线下面积分别是0.82和0.76(95%CI:0.75~0.88和0.69~0.83)。见表 2和图 1。
| 表 2 丙球治疗前后NLR、PLR对于川崎病IVIG敏感性的预测价值 |
|
图 1 丙球治疗前后的NLR、PLR对于川崎病IVIG敏感性预测的ROC曲线 |
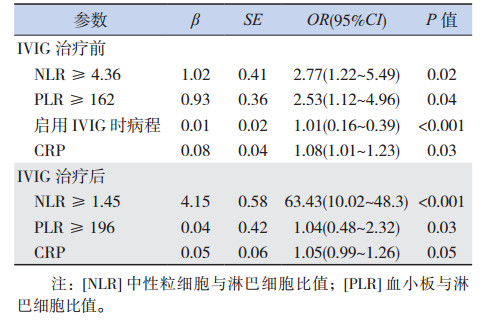
2.3 川崎病IVIG不敏感的危险因素
多元回归分析显示,IVIG治疗前NLR≥4.36和PLR≥162,IVIG治疗后NLR≥1.45和PLR≥196是IVIG不敏感的有效预测因素;在病程早期越早使用IVIG越有可能发生IVIG不敏感;IVIG治疗前的CRP越高越有可能发生IVIG不敏感。见表 3。
| 表 3 川崎病IVIG不敏感的危险因素logistic回归分析 |
3 讨论
NLR是炎症反应和免疫平衡的反映[5]。研究报道休克和脓毒症的病情严重程度与中性粒细胞增多、淋巴细胞减少有关[4]。因此,NLR增高可视为炎症反应加剧的标志。Sato等[17]认为,川崎病急性期中性粒细胞数量增加,嗜中性粒细胞弹性蛋白酶和髓过氧物酶增加,导致组织自我破坏,因此中性粒细胞百分比增高可作为丙球抵抗的预测指标。Kawamura等[13]研究也证实,NLR可作为川崎病患者丙球不敏感的独立危险因素。本研究显示,不论是丙球治疗前还是丙球治疗后,丙球不敏感组的NLR均明显高于丙球敏感组,NLR可作为川崎病患者丙球不敏感的危险因素。
PLR是血小板与淋巴细胞的比值,是十分重要的系统性炎症标志物和心血管不良事件的预测指标[7-8]。在系统性感染和炎症的情况下,促炎细胞活素水平增高刺激巨核细胞增殖,导致血小板计数增高。本研究显示,IVIG不敏感组的PLR明显高于敏感组,PLR可作为IVIG敏感性的预测指标。
川崎病是儿童后天性心脏病的主要病因,主要危害为冠状动脉扩张及冠状动脉瘤形成[18]。而IVIG不敏感川崎病患者冠状动脉扩张的风险明显增高[19]。因此早期预测川崎病IVIG敏感性对治疗方案的选择及预后评估起到指导意义。本研究显示,川崎病患儿IVIG治疗前、后的NLR和PLR对IVIG不敏感的最佳预测值分别为4.36、162和1.45、196。但要实现NLR和PLR对于川崎病的临床指导作用,还需进一步的大规模、多中心研究。
| [1] | McCrindle BW, Li JS, Minich LL, et al. Coronary artery involvement in children with Kawasaki disease:risk factors from analysis of serial normalized measurements[J]. Circulation, 2007, 116 (2): 174–179. DOI:10.1161/CIRCULATIONAHA.107.690875 |
| [2] | Ha KS, Lee J, Jang GY, et al. Value of neutrophil-lymphocyte ratio in predicting outcomes in Kawasaki disease[J]. Am J Cardiol, 2015, 116 (2): 301–306. DOI:10.1016/j.amjcard.2015.04.021 |
| [3] | Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease:a statement for health professionals from the committee on rheumatic fever, endocarditis and Kawasaki disease, council on cardiovascular disease in the Young, American Heart Association[J]. Circulation, 2004, 110 (17): 2747–2771. DOI:10.1161/01.CIR.0000145143.19711.78 |
| [4] | Hwang SY, Shin TG, Jo IJ, et al. Neutrophil-to-lymphocyte ratio as a prognostic marker in critically-ill septic patients[J]. Am J Emerg Med, 2017, 35 (2): 234–239. DOI:10.1016/j.ajem.2016.10.055 |
| [5] | Azab B, Zaher M, Weiserbs KF, et al. Usefulness of neutrophil to lymphocyte ratio in predicting short-and long-term mortality after non-ST-elevation myocardial infarction[J]. Am J Cardiol, 2010, 106 (4): 470–476. DOI:10.1016/j.amjcard.2010.03.062 |
| [6] | Park JJ, Jang HJ, Oh IY, et al. Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Am J Cardiol, 2013, 111 (5): 636–642. DOI:10.1016/j.amjcard.2012.11.012 |
| [7] | Acet H, Ertas F, Akıl MA, et al. Relationship between hematologic indices and global registry of acute coronary events risk score in patients with ST-segment elevation myocardial infarction[J]. Clin Appl Thromb Hemost, 2016, 22 (1): 60–68. DOI:10.1177/1076029614533145 |
| [8] | Lian L, Xia YY, Zhou C, et al. Application of platelet/lymphocyte and neutrophil/lymphocyte ratios in early diagnosis and prognostic prediction in patients with resectable gastric cancer[J]. Cancer Biomark, 2015, 15 (6): 899–907. DOI:10.3233/CBM-150534 |
| [9] | Çiçek G, Açıkgoz SK, Bozbay M, et al. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio combination can predict prognosis in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. Angiology, 2015, 66 (5): 441–447. DOI:10.1177/0003319714535970 |
| [10] | Cummings M, Merone L, Keeble C, et al. Preoperative neutrophil:lymphocyte and platelet:lymphocyte ratios predict endometrial cancer survival[J]. Br J Cancer, 2015, 113 (2): 311–320. DOI:10.1038/bjc.2015.200 |
| [11] | Kobayashi T, Inoue Y, Takeuchi K, et al. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease[J]. Circulation, 2006, 113 (22): 2606–2612. DOI:10.1161/CIRCULATIONAHA.105.592865 |
| [12] | Kim T, Choi W, Woo CW, et al. Predictive risk factors for coronary artery abnormalities in Kawasaki disease[J]. Eur J Pediatr, 2007, 166 (5): 421–425. DOI:10.1007/s00431-006-0251-8 |
| [13] | Kawamura Y, Takeshita S, Kanai T, et al. The combined usefulness of the neutrophil-to-lymphocyte and platelet-tolymphocyte ratios in predicting intravenous immunoglobulin resistance with Kawasaki disease[J]. J Pediatr, 2016, 178 : 281–284.e1. DOI:10.1016/j.jpeds.2016.07.035 |
| [14] | Yim D, Curtis N, Cheung M, et al. An update on Kawasaki disease Ⅱ:clinical features, diagnosis, treatment and outcomes[J]. J Paediatr Child Health, 2013, 49 (8): 614–623. DOI:10.1111/jpc.2013.49.issue-8 |
| [15] | 《中华儿科杂志》编辑委员会, 中华医学会儿科学分会心血管学组, 中华医学会儿科学分会免疫学组. 川崎病专题讨论会纪要[J]. 中华儿科杂志, 2007, 45 (11): 826–830. DOI:10.3760/j.issn:0578-1310.2007.11.007 |
| [16] | Research Committee of Kawasaki Disease. Report of subcommittee on standardization of diagnostic criteria and reporting of coronary artery lesions in Kawasaki disease[S]. Tokyo, Japan:Ministry of Health and Welfare, 1984. |
| [17] | Sato S, Kawashima H, Kashiwagi Y, et al. Inflammatory cytokines as predictors of resistance to intravenous immunoglobulin therapy in Kawasaki disease patients[J]. Int J Rheum Dis, 2013, 16 (2): 168–172. DOI:10.1111/apl.2013.16.issue-2 |
| [18] | Daniels LB, Tjajadi MS, Walford HH, et al. Prevalence of Kawasaki disease in young adults with suspected myocardial ischemia[J]. Circulation, 2012, 125 (20): 2447–2453. DOI:10.1161/CIRCULATIONAHA.111.082107 |
| [19] | Adachi S, Sakaguchi H, Kuwahara T, et al. High regression rate of coronary aneurysms developed in patients with immune globulin-resistant Kawasaki disease treated with steroid pulse therapy[J]. Tohoku J Exp Med, 2010, 220 (4): 285–290. DOI:10.1620/tjem.220.285 |
 2017, Vol. 19
2017, Vol. 19