患儿,男,14岁,因腹痛12 d入院。患儿腹痛呈脐周及上腹部阵发性疼痛,程度不剧烈,呕吐胃内容物1次,无发热,无皮肤、巩膜黄染,无腹泻、黑便等。至当地医院就诊,查血淀粉酶225 U/L(参考值:0~100 U/L),血脂肪酶1 506 U/L(参考值:13~60 U/L);血常规:白细胞16.48×109/L,中性粒细胞82.7%,余项正常;C反应蛋白(CRP)117 mg/L;腹部B超提示胰腺增大伴回声改变,胰周低弱回声团,盆腔积液;磁共振胰胆管成像(MRCP)提示胰管扩张,胰头部胰管显示不清,胆囊增大。当地医院考虑“急性胰腺炎”,予禁食、补液、抗感染、奥美拉唑、生长抑素等对症支持治疗,住院期间出现发热伴轻微咳嗽,抗感染治疗后患儿体温恢复正常,但仍有上腹部疼痛。既往史、个人史、家族史无特殊。
入院体查:生命体征平稳,体质指数(BMI)24.1 kg/m2,神清,精神差,急性病容,皮肤、巩膜无黄染,颈部、腋下、腹股沟浅表淋巴结未触及,两肺听诊呼吸音对称、清晰,未闻及罗音,腹软,脐周及上腹部压痛,无反跳痛,肝脾肋下未及,腹部移动性浊音阴性,双下肢无浮肿,神经系统检查阴性。
辅助检查:血常规白细胞21.92×109/L,中性粒细胞比值87.5%,余项正常;C反应蛋白111 mg/L;肝功能正常;血淀粉酶正常,脂肪酶71.1 U/L(参考值:13~60 U/L);乳酸脱氢酶386 U/L(参考值:110~295 U/L)。腹部B超:胰腺外形饱满、边缘模糊,胰管扩张(内径约0.45 cm),胰头周围淋巴结肿大(较大者直径约3.2 cm×2.3 cm)、边界尚清、其内回声减低、尚均匀,腹腔积液、胸腔积液。肺部CT:两肺散在结节影。真菌D-葡聚糖:13.468 pg/mL(参考值:< 10 pg/mL);结核感染T细胞斑点试验(T-spot)阴性。
2 诊断思维本例患儿无明显诱因出现急性上腹痛,血淀粉酶及脂肪酶高于正常上限三倍,白细胞增高、中性粒细胞增高,C反应蛋白增高,影像学提示胰腺增大、胰管扩张,可临床诊断急性胰腺炎。细菌、病毒、寄生虫等引起的胆道感染均可导致急性胰腺炎;先天性胰胆管异常如胆总管囊肿、胰腺分裂可引起胰腺炎;胆道结石、胆道蛔虫症所致的胆管梗阻,以及腹部外伤、过敏性紫癜、系统性红斑狼疮、炎症性肠病、川崎病等全身性疾病均可伴发胰腺炎;毒物、药物,内分泌疾病如高钙血症、高脂血症,以及遗传代谢病也可能是儿童急性胰腺炎的病因[1]。本例患儿无其它全身性疾病的临床表现,无特殊用药史,既往、个人史无特殊,血常规提示白细胞、中性粒细胞升高,CRP显著升高,实验室检查未提示高血钙、高血脂。因此,考虑胆道细菌感染引起的急性胰腺炎可能性大。但抗感染、制酸、抑制胰酶分泌治疗效果欠佳,而且胰腺B超提示胰头周围淋巴结肿大、胰管扩张,MRCP提示胰腺头部显示不清,需注意淋巴瘤等肿瘤压迫所致,进一步复查腹部CT及MRCP,并行腹腔淋巴结活检明确诊断。
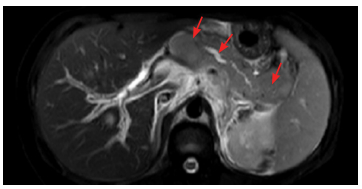
3 进一步检查MRCP(图 1)提示:胰腺外形饱满,边界不清,胰周、脾周、左侧肾周间隙及胆囊窝积液,肝门部及后腹膜融合肿大淋巴结。腹部CT:胰腺肿胀、胰腺内多处低密度灶,伴胰管扩张、胰周渗出,肝门部及后腹膜淋巴结肿大。行腹腔镜探查,发现:肝门部多发结节、水肿明显,与周围结构分界不清,胰腺水肿严重。转为剖腹探查可见:胰腺水肿严重,未见明显占位,肝门部多发结节、伴明显水肿、与周围结构分界不清,取肝门部结节及大网膜肿大淋巴结行病理检查。淋巴结病理:淋巴结结构破坏,间变大细胞成片分布;免疫组化:EMA+,Desmin-,CK散在+,Vim+,CD20散在+,CD3局部+,INI-1+,MPO-,ALK+,CD30+,MyoD1-,Ki-67约97%+;诊断(肝门、胃大弯网膜)间变大细胞淋巴瘤。骨髓细胞学及流式细胞检查正常,脑脊液检查正常。PET/MRI提示弥漫性胰腺恶性淋巴瘤。
|
图 1 患儿的MRCP表现 MRCP可见胰腺肿胀明显,胰腺内多处低密度灶、以胰头处病变最大,伴胰管明显扩张。如箭头所示。 |
诊断:原发性胰腺淋巴瘤(primary pancreatic lymphoma, PPL)(间变大细胞淋巴瘤)Ⅲ期,急性胰腺炎。PPL诊断依据:(1)腹痛、呕吐,肝门及腹膜后淋巴结肿大;(2)无肝脾侵犯,无骨髓及中枢受累;(3)腹腔病变不能手术切除;(4)淋巴结活检病理提示间变大细胞淋巴瘤。
5 临床经过患儿经抗感染、制酸、抑制胰酶分泌治疗病情仍进展,迅速发生脓毒症、脓毒性休克,并出现多脏器功能衰竭。转入重症监护室,予气管插管、呼吸机支持辅助通气。病理初步诊断为淋巴瘤后,予以VD方案(长春地辛、地塞米松)减轻肿瘤负荷,继续对症支持治疗,患儿肺部感染控制、腹痛好转,血淀粉酶降至正常,逐渐恢复饮食,并脱离呼吸机;考虑患儿因病变范围广且胰腺炎症状好转,予以VDLD(长春地辛、吡柔比星、门冬酰胺酶、地塞米松)方案化疗,第一次门冬酰胺酶应用后患儿再次出现腹痛、血淀粉酶升高至1 600 U/L,再次予禁食、抑酸、抑酶治疗后腹痛症状好转、血淀粉酶降至轻度升高。以后予以长春瑞滨(每周一次,8次)+地塞米松化疗,继续空肠营养及静脉营养,血淀粉酶反复波动,并且多次复查影像学仍有腹腔淋巴结肿大及胰腺低密度病灶。应用第8次长春瑞滨后复查胰腺B超仍提示胰头低密度灶及腹腔淋巴结肿大,患儿家长放弃治疗。
6 讨论非霍奇金淋巴瘤是儿童最常见的肿瘤之一,可以累及结外以及实质性脏器,约三分之一可累及胰腺。PPL约占结外淋巴瘤的1%,发病年龄以50~60岁常见,儿童罕见[2]。PPL起源于胰腺或仅侵犯胰腺及其区域淋巴结,无肝脾肿大,无浅表及纵膈淋巴结肿大[3]。PPL病因不明,可能与遗传、免疫缺陷、疱疹病毒、肝炎病毒等病毒感染等有一定关系[4]。成人PPL或转移性肿瘤侵犯胰腺引发胰腺炎,以及儿童胰腺淋巴瘤引起胰腺炎均极其罕见,仅有少量国外文献报道[5]。本研究患儿以胰腺炎为表现,影像学提示胰腺肿胀、胰腺内多发低密度病灶、肝门及腹膜后淋巴结肿大,淋巴结病理提示间变大细胞淋巴瘤。
PPL临床表现无特异性,可表现为腹痛、恶心、呕吐及发热、体重下降等,如肿块压迫胆管可有梗阻性黄疸表现。部分患者有血清淀粉酶、脂肪酶、乳酸脱氢酶升高,而肿瘤标志物CA 199一般正常,伴胆管梗阻时可轻度升高。部分患儿无明显临床症状仅在影像学检查时偶然发现。胰腺CT或MRI表现为低密度均匀回声包块,以单发病灶多见,位置以胰头最常见。包块因生长迅速,体积一般较大,胰腺淋巴瘤一般直径大于6 cm,而胰腺癌直径一般小于6 cm,呈分叶状,周围胰腺组织强化明显[2]。个别PPL病变为多灶性分布或弥漫性分布,胰腺呈弥漫性肿大[5]。本例患儿的影像学未发现单发占位,提示弥漫性胰腺肿大、多处低密度病灶,考虑多灶性病变。PPL确诊主要依靠病理,如超声内镜细针穿刺、腹腔镜肿块或淋巴结活检明确。国外文献报道[2, 6-15]的PPL中,14例儿童PPL的病理类型以Burkitt淋巴瘤最常见(9例),还包括3例弥漫大B细胞淋巴瘤、2例间变细胞淋巴瘤,而成人PPL以弥漫大B细胞淋巴瘤为主,除2例未说明预后、1例仍在化疗中,其余患者化疗后临床症状及影像学缓解。
PPL的治疗与淋巴瘤的病理分型和临床分期有关,文献报道[2, 6-15]大部分儿童PPL通过单纯化疗长期缓解率较高(其病理以Burkitt淋巴瘤和弥漫大B细胞淋巴瘤为主,分期多在Ⅰ期和Ⅱ期)。PPL一线化疗用药包括泼尼松龙、长春新碱、阿霉素以及环磷酰胺等[16]。对于CD20阳性的弥漫大B细胞淋巴瘤,利妥昔单抗可以增加疗效[17]。放疗并没有证实能增加PPL疗效[18]。PPL往往因肿块较大或与正常组织分界不清,胰瘘发生率高,手术治疗较困难[19]。本例患者病理提示间变大细胞淋巴瘤,临床进展快,全身情况差,淋巴结活检初步诊断淋巴瘤后予VD方案减轻瘤负荷,胰腺炎症状控制,予VDLD方案化疗,一次门冬酰胺酶后胰腺炎症状复发,因此对于肿瘤侵犯或者压迫胰胆管导致胰腺炎的PPL患者应慎用门冬酰胺化疗。虽然文献报道大部分儿童PPL通过单纯化疗长期缓解率较高,但对于急性胰腺炎表现、全身情况较差的患者如何结合病理分型、临床分期采取最佳治疗仍需进一步研究。
7 结语本例患者临床表现为急性胰腺炎,影像学检查发现腹腔淋巴结肿大,经淋巴结活检病理证实为间变大细胞淋巴瘤,PPL为儿童急性胰腺炎的罕见病因。对于疗效不佳、症状反复的急性胰腺炎患者需注意少见病因,尤其是合并腹腔淋巴结肿大伴有乳酸脱氢酶明显增高时,需警惕结外淋巴瘤,尽早进行病理诊断。儿童胰腺淋巴瘤罕见,是否需要手术治疗缺乏经验;而对于有胰腺炎表现者,门冬酰胺酶的使用需谨慎。对于以急性胰腺炎表现的儿童PPL的治疗仍值得进一步探索,尤其是侵袭性较强的间变大细胞淋巴瘤。
| [1] |
Husain SZ, Srinath AI. What's unique about acute pancreatitis in children:risk factors, diagnosis and management[J]. Nat Rev Gastroenterol Hepatol, 2017, 14(6): 366-372. DOI:10.1038/nrgastro.2017.13 (  0) 0) |
| [2] |
Yoon WJ, Yoon YB, Kim YJ, et al. Primary pancreatic lymphoma in Korea——a single center experience[J]. J Korean Med Sci, 2010, 25(4): 536-540. DOI:10.3346/jkms.2010.25.4.536 (  0) 0) |
| [3] |
Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract.Report of 37 cases with a study of factors influencing prognosis[J]. Br J Surg, 1961, 49: 80-89. DOI:10.1002/(ISSN)1365-2168 (  0) 0) |
| [4] |
Loots E, Anderson F, Thomson SR. Primary pancreatic lymphoma in an HIV patient:dilemmas in diagnosis and management[J]. S Afr J Surg, 2008, 46(1): 28-29. (  0) 0) |
| [5] |
Koca T, Aslan N, Dereci S, et al. Burkitt lymphoma with unusual presentation:Acute pancreatitis[J]. Pediatr Int, 2015, 57(4): 775-777. DOI:10.1111/ped.2015.57.issue-4 (  0) 0) |
| [6] |
Eisenhuber E, Schoefl R, Wiesbauer P, et al. Primary pancreatic lymphoma presenting as acute pancreatitis in a child[J]. Med Pediatr Oncol, 2001, 37(1): 53-54. DOI:10.1002/(ISSN)1096-911X (  0) 0) |
| [7] |
Amodio J, Brodsky JE. Pediatric Burkitt lymphoma presenting as acute pancreatitis:MRI characteristics[J]. Pediatr Radiol, 2010, 40(5): 770-772. DOI:10.1007/s00247-009-1475-3 (  0) 0) |
| [8] |
Shapira G, Fisher Y, Ilivitzki A. Bifocal primary pancreatic Burkitt's lymphoma in a 4-year-old child[J]. J Clin Ultrasound, 2017, 45(3): 171-174. DOI:10.1002/jcu.v45.3 (  0) 0) |
| [9] |
Nasher O, Hall NJ, Sebire NJ, et al. Pancreatic tumours in children:diagnosis, treatment and outcome[J]. Pediatr Surg Int, 2015, 31(9): 831-835. DOI:10.1007/s00383-015-3727-7 (  0) 0) |
| [10] |
Park M, Koh KN, Kim BE, et al. Pancreatic neoplasms in childhood and adolescence[J]. J Pediatr Hematol Oncol, 2011, 33(4): 295-300. DOI:10.1097/MPH.0b013e318206990a (  0) 0) |
| [11] |
Pietsch JB, Shankar S, Ford C, et al. Obstructive jaundice secondary to lymphoma in childhood[J]. J Pediatr Surg, 2001, 36(12): 1792-1795. DOI:10.1053/jpsu.2001.28840 (  0) 0) |
| [12] |
Sood V, Agrawal N, Alam S, et al. Primary pancreatic lymphoma simulating acute cholestatic hepatitis in a 7-year-old child[J]. ACG Case Rep J, 2015, 2(3): 190-192. (  0) 0) |
| [13] |
Fraser CJ, Chan YF, Heath JA. Anaplastic large cell lymphoma of the pancreas:a pediatric case and literature review[J]. J Pediatr Hematol Oncol, 2004, 26(12): 840-842. (  0) 0) |
| [14] |
Araújo J, Sampaio MC, Sousa L. Pancreas Burkitt primary lymphoma in pediatric age[J]. Rev Esp Enferm Dig, 2017, 109(6): 451. (  0) 0) |
| [15] |
Meier C, Kapellen T, Tröbs RB, et al. Temporary diabetes mellitus secondary to a primary pancreatic Burkitt lymphoma[J]. Pediatr Blood Cancer, 2006, 47(1): 94-96. DOI:10.1002/(ISSN)1545-5017 (  0) 0) |
| [16] |
Du X, Zhao Y, Zhang T, et al. Primary pancreatic lymphoma:a clinical quandary of diagnosis and treatment[J]. Pancreas, 2011, 40(1): 30-36. DOI:10.1097/MPA.0b013e3181e6e3e5 (  0) 0) |
| [17] |
Alexander RE, Nakeeb A, Sandrasegaran K, et al. Primary pancreatic follicle center-derived lymphoma masquerading as carcinoma[J]. Gastroenterol Hepatol (N Y), 2011, 7(12): 834-838. (  0) 0) |
| [18] |
Serin KR, Guven K, Özden I, et al. Curative Chemoradiotherapy of Primary Pancreatic Lymphoma with Vertebral Metastasis:Palliation of Persistent Biliary Stricture by Roux-en-Y Hepaticojejunostomy[J]. Case Rep Gastroenterol, 2011, 5(3): 642-647. DOI:10.1159/000334725 (  0) 0) |
| [19] |
Koniaris LG, Lillemoe KD, Yeo CJ, et al. Is there a role for surgical resection in the treatment of early-stage pancreatic lymphoma?[J]. J Am Coll Surg, 2000, 190(3): 319-330. DOI:10.1016/S1072-7515(99)00291-4 (  0) 0) |
 2018, Vol. 20
2018, Vol. 20


