2. Department of Respiratory and Critical Care Medicine, Second Affiliated Hospital of Fujian Medical University, Quanzhou, Fujian 362000, China
The possibility to ventilate independently one or both lungs -one-lung ventilation (OLV) and independent-lung ventilation (ILV) -can be required in intensive care, in general anesthesia, and in the postoperative care of all pediatric patients.
While for the adult the Carlen's double-lumen tube (DLT) has largely solved the technical problem that arises for selective bronchial intubation (SBI), for pediatric patients and especially for children below 6-8 years of age technical difficulties remain due to the unavailability of suitable DLTs. Bronchial blockers or conventional single lumen tubes have been proposed and are used for SBI and OLV in infants and younger children. The main limits of bronchial blockers and single lumen tube are:not easy collapse and reexpansion of the lung if required; easy dislodgement during the treatment; and frequent need of fiberscope for appropriate positioning.
The demand for greater flexibility in the ventilation during general anesthesia increased with the development of video assisted thoracoscopy surgery, and SBI and OLV have become important procedures to facilitate the surgery. But SBI remains still an open problem due to the difficulty of having on the market appropriate devices for the selective intubation of newborns, infants and younger children[1].
Since the first application in the treatment of lung disease in intensive care in the late 1980s, the separate lung ventilation for the treatment of lung pathologies with unilateral prevalence has encouraged the indication of ILV in the post-operative care (i.e. post cardio-thoracic surgery). In this context ILV can play an important role in the prevention of postoperative lung complications so far as lung areas not perfectly re-ventilated can persist at the end of anesthesia. Not complete lung re-expansion and postoperative atelectasis are called into question in the origin of post-operative pneumonia and consequently in the final outcome of the surgery.
The limitations in the use of ILV in intensive care still remain due to the lack of suitable DLTs useful for all pediatric ages, for the need to use two synchronized ventilators, and for the complexity of the treatment[2].
The arrival of the "Marraro Paediatric Endobronchial Bilumen Tube®" (mPEBT) opened large hopes both in anesthesia and intensive care because it allowed the treatment of children from neonates to 4-5 years of age[3-4].
1 SBISBI is the possibility of intubating selectively a single main bronchus in order to perform ventilation in only one lung. SBI can be done using DLTs in adolescents and children over 6-8 years of age similar to those used in adults. In neonates and younger children SBI can be done only using bronchial blockers and single lumen tube due to the lack of suitable DLTs. In these age groups only OLV is possible.
1.1 OLVOLV, also known as single lung ventilation, means the possibility to ventilate only one lung while the other is kept unventilated or collapsed. The ventilation of one lung is frequently required in general anesthesia for cardio-thoracic surgery because allows the possibility to ventilate only one lung and exclude the contralateral to the ventilation favouring the surgery.
OLV is indicated in intensive care for the treatment of pneumothorax which does not resolve with the application of thoracic drainage, in tracheobronchial fistula, in lung hemorrhage that affects only one lung, when is necessary to keep one lung separate from the other, i.e. to avoid the spread of unilateral lung pathology (hemorrhage, infection) to both lungs, and for recruitment lung maneuvers.
OLV is well tolerated when the excluded lung is completely collapsed and perfusion is absent. If the lung is not completely excluded from ventilation and perfusion, hypoxia and hypercapnia can occur.
1.2 ILVILV allows the isolation of one lung from the other and favors the ventilation of both lungs separately. Different ventilation models, tidal volume and levels of positive end-expiratory pressure (PEEP) can be applied to each lung. ILV can only be done through the use of a DLT or two single lumen tubes, positioned one in the trachea and the other in a main bronchus.
Right and left SBI can be performed but the selective left bronchial intubation is preferred because right main bronchus intubation exposes to the risk of exclusion to ventilation of the upper right lobe favouring the development of atelectasis.
ILV is indicated in unilateral lung disease, bilateral lung pathology complicated by unilateral atelectasis, pneumothorax, tracheo-bronchial fistula, and to avoid the diffusion of contamination or bleeding from one lung to the contralateral. In the post-operative care is useful to re-expand and keep open the lung collapsed and/or manipulated during surgery. ILV can be used also for lung recruitment, selective broncho-alveolar lavage, selective surfactant supplementation and for local drug application[5-7].
2 Methods to achieve SBIOLV and ILV can be carried out mainly using three devices:double-lumen endobronchial tube, bronchial blockers and single-lumen endotracheal tube (ETT)[8-11].
Anatomical characteristic of pediatric airways and recommended devices for SBI, OLV and ILV in pediatric age, according to the devices available on the market, are described in Table 1.
| 表 1 Characteristic of pediatric airways and available devices for SBI, OLV and ILV |
|
|
The double-lumen endobronchial tube allows access to the two lungs separately in order to apply different ventilation modes and different PEEP levels to each lung, to collapse and exclude one lung to the ventilation, to avoid the spread of infection or hemorrhage from one lung to the other.
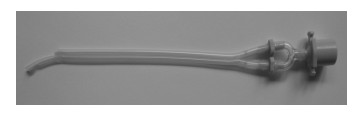
Over 6-8 years of age, SBI is possible using DLTs similar to that used in adults (Bronchocath Mallinckrodt® and Bronchoport Rusch®) (Figure 1).

|
图 1 Mallinckrodt® double-lumen tube without carinal hook useful for selective bronchial intubation in children over 6-8 years of age |
Adult DLTs are available for both right and left SBI. In principle, the left-sided and right-sided DLTs should be similarly safe and efficacious. However, in fact, the use of the right-sided DLT is controversial due to the high risk of excluding to ventilation the upper lobe of the right lung and consequently to the development of atelectasis[12-13].
No single predictor can determine which size of DLT can be used at different pediatric ages. The best predictor to estimate the size of a DLT is the tracheal width highlighted from the posterior-anterior chest X-ray[14].
The positioning of the DLT can be done under direct laryngoscopy and/or by the flexible fiberscope.
In the early 1990s the development of the mPEBT has allowed the possibility to carry out SBI and synchronized ILV in neonates and infants below 4-5 years of age[4]. The mPEBT is currently available only as special product.
The mPEBT consists of two separate uncuffed tubes of different length, attached laterally to each other. This DLT is made in medical grade polyvinyl chloride (PVC), has no spur for anchoring to the carina and presents for its entire length a radiopaque blue line for radiological visualization (Figures 2 and 3)[4].

|
图 2 mPEBT with separate connectors to ventilate the two lungs individually with two ventilators |
|
图 3 The same double-lumen tube of Figure 2 with a single connector to ventilate both lungs at the same time with only one ventilator |
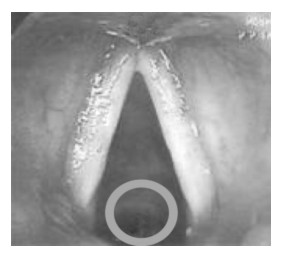
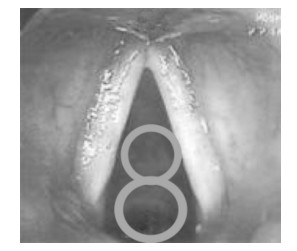
Different sizes of mPEBT are suitable for treating neonates, infants and children up to 4-5 years[15]. It is possible to use an mPEBT tube of larger diameter than would be supposed because the two branches of the tube after positioning are allocated one above the other between the vocal cords (Figures 4 and 5).
|
图 4 Position of single lumen tube of 3 mm internal diameter through the vocal cords |
|
图 5 Position of the mPEBT through the vocal cords The two lumens, 3 mm and 2.5 mm, are one over the other. |
The insertion of mPEBT takes place under direct laryngoscopy and normally does not need the use of fiberscope. The absence of cuffs allows the use of tubes of a larger size but the applied PEEP level could be unstable for the possible leakage. If a high level of PEEP is applied in the selectively intubated lung, the leakage that is achieved does not allow to keep different PEEP levels in each lung.
There are several evaluation methods to confirm the correct SBI including lung auscultation, selective capnography (EtCO2), fiberoptic visualization, and chest X-ray[16-19].
2.2 Bronchial blockersBronchial blockers are special devices designed to be placed in the airway through or alongside the conventional ETT. Different types of bronchial blockers are available and can be used for SBI and represent an alternative when suitable DLTs are not available or cannot be positioned.
Bronchial blockers can essentially be classified into two main groups.
First group:includes catheters used for embolectomy, arterioseptomy and cardiac catheterization. They are used as "off-label" because they are originally designed and intended for other clinical purposes[20-24]. These bronchial blockers are the choice of option when DLTs are not available for all pediatric ages.
These catheters have an inflatable balloon-cuff at distal end. The cuff has low-volume and high-pressure properties without any possibility of progressive inflation. This characteristic increases the risk of ischemia of the bronchial mucosa.
Fogarty embolectomy catheter do not have a central lumen useful for bronchial suctioning and oxygen supplementation. Central lumen is present in arterioseptostomy and pulmonary artery catheters. Arterioseptostomy catheter presents also a special angled tip that can favor the bronchial positioning. Due to the specific characteristics, it is the one that is most used in clinical practice.
These blockers if positioned through the ETT increases the resistance to the gas flow and may cause difficulty in ventilation.
The correct positioning of these bronchial blockers can be confirmed by simple auscultation of both lungs but preferentially with fiberoptic bronchoscopy.
Second group:includes devices which incorporate a dedicated blocker channel within the wall of the tube. The blocker has incorporated a highvolume, low-pressure cuff at the tip. It is necessary to use fiberoptic guidance to confirm proper device placement.
Wire-guided endobronchial Arndt blocker®, UniventTM tube and UniblockerTM are used as bronchial blockers for SBI in older children. Cohen® Flexitip Endobronchial Blocker, CoopdechTM endobronchial blocker tube, EZ-blockerTM and Papworth BiVent ETT are available for adults but their use in pediatric age has not been demonstrated[25-27].
Wire-guided endobronchial Arndt blocker® is a bronchial blocker with a central lumen, through which a wire with a looped end can be pass for fixing the blocker to the tip of fiberscope and subsequently positioned in one main bronchus.
This blocker is available in 3 sizes:5 Fr, 7 Fr, and 9 Fr. Size 9 Fr is recommended for ETTs of 7.5 mm and above; 7 Fr for ETTs of 6.0 to 7.0 mm; and 5 Fr for ETTs of 4.5 to 5.5 mm. A new extra-luminal 5 Fr Arndt blocker® is available and suggested to overcome the traditional limit of its use below 6 years of age[11].
UniventTM tube is a standard single lumen tracheal tube, cuffed and uncuffed, with an additional internal lumen incorporating a movable blocker that can be advanced into a bronchus. The internal diameter (ID) of the ETT is smaller compared the total outer diameter of entire tube which results in high resistance to gas flow (Figure 6). UniventTM tube with 3.5 mm ID has an external total cross-sectional diameter of 7.5-8.0 mm which makes it unusable in children.

|
图 6 Cuffed and uncuffed UniventTM tube useful for children over 8-10 years of age |
The UniventTM tube has a central channel, useful for favoring the collapse of the lung, for bronchosuction and to insufflate oxygen into the lung. The blocker can be withdrawn from the bronchus allowing the possibility to ventilate both lungs contemporarily. In post-operative ventilation, the bronchial blocker can be removed and the tube can be left in place like a standard ETT.
The placement of Univent tubeTM can be critical and can require the use of flexible fiberscope and skilled and experienced operators[28].
The most commonly encountered complications with all types of bronchial blockers are the failure to SBI, the dislodgment of the blocker from the selected bronchus, the proximal herniation of the cuff at level of tracheal carina (particularly during patient positioning), the failure to achieve lung separation because of abnormal anatomy, and accidental breakage of the cuff. These complications can lead to severe hypoxemia if not immediately recognized and appropriately treated. Repositioning of a problematic blocker can be difficult and frequently requires fiberoptic guidance to solve the problem.
2.3 Single-lumen endobronchial tubeEndobronchial intubation using a normal or modified single-lumen ETT for lung isolation was described in the early 1930s. This method, using conventional or special cuffed or uncuffed ETT, is still applied in neonates and infants due to the sufficient length of the tubes when appropriate DLT or bronchial blockers are not available.
Modified ETTs, microlaryngeal tubes, available in three sizes, 4.0, 5.0 and 6.0 mm ID, can be used in all children when conventional tubes have not sufficient length to obtain selective intubation.
SBI using a conventional ETT is favored placing the child in semi-lateral posture that accentuates the anatomic location of the bronchi (i.e. raising the shoulder opposite to the bronchus to be intubated) and/or using fiberscope.
The suitable ETT is advanced into the trachea and progressively in the left or right main bronchus. The correct position is confirmed by auscultation of the ventilation only in the selectively intubated lung and absence of ventilation to the contralateral lung. Using uncuffed tube is difficult to obtain complete adequate bronchial seal.
The ETT can be easily withdrawn from the bronchus into the trachea allowing the immediate possibility of ventilating both lungs. The return to bilateral lung ventilation does not allow the appropriate re-expansion of both lungs due to the change of compliance and resistance of the collapsed/ non ventilated lung.
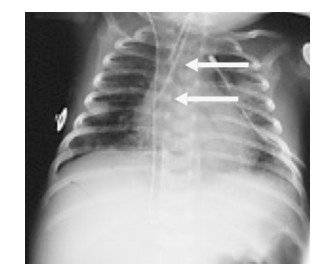
Two conventional tubes can be used in clinical practice for SBI and ILV in neonates and younger infants. One tube is positioned into one main bronchus for obtaining the SBI and the other is kept into the trachea to ventilate the contralateral lung (Figures 7 and 8). Generally, nasal intubation is preferred because allows a better stability of the tubes and reduces the risk of dislodgement. The method can be helpful if suitable DLT is not available and ILV is indicated.

|
图 7 One month old baby treated with independent-lung ventilation using two single uncuffed tubes for the treatment of pneumothorax not resolved with conventional drainage treatment |
|
图 8 The chest X-ray of the same case to Figure 7 shows an endotracheal tube positioned in the trachea (upper arrow) while the other is placed in the right bronchus (lower arrow). |
The positioning of a single lumen uncuffed tube via tracheostomy for endobronchial intubation and another positioned nasally in the trachea for ventilation of contralateral lung has been recently described in literature with successful result[29].
Advantages, disadvantages and limitation in the use of the different technique of SBI are illustrated in Table 2.
| 表 2 Advantages, disadvantages and limitations of selective endobronchial devices |
|
|
In case of severe difficulty in ventilation and need for re-positioning of the ETT, DLT and/or a bronchial blocker, it is necessary to remove the applied device, ventilate the patient using a bag and mask, and when oxygenation has normalized proceed to a new SBI attempt. Frequently the previously positioned device cannot be used for the second attempt.
Severe airway injuries during OLV as subcutaneous emphysema, inflammatory and mechanical injury[30], and acquired bronchial stenosis[31] are rare occurrence. Unexpected air leak and pneumothorax, airway bleeding or protrusion of the endotracheal or endobronchial cuff into the surgical field are very rare complications. If any of these complications occurs, a bronchoscopy must be immediately performed and appropriate treatment must be applied.
3 Considerations to improve safety and reduce complications using medical devicesGreat attention is currently being paid to treatments received by infants and children in intensive care (NICU and PICU), in anesthesia, and in surgery in order to address issues of safety and quality of care. There are intrinsic risk and potential complications associated with the use of biomedical products and/or introduction of new devices in the clinical practice if they are not appropriately experimented[32].
Medico-legal issues often derive from disagreement over the timeliness or appropriateness of diagnosis and treatment, which includes the prevention of harm from critical care procedures. Complying with protocols for clinical treatments in critical care and anesthesia of pediatric patients can contribute to reduce mobility, mortality and the risk of medicallegal issues[33-34].
Selective bronchial intubation is a crucial methodology that can be indicated in intensive care, in general anesthesia, during and after surgery, in postoperative care of infants and children.
All the methods to achieve SBI in infants and younger children are complex and require adequate knowledge and specific technical skills. Improvisation in performing SBI must be avoided because expose at risk of severe complications. Specific advantages, disadvantages, limitations of SBI and different devices to be used must be carefully evaluated before, during and after the treatment, taking into account the anatomical and physiological characteristics of pediatric patients, the experience of physicians and nurses team in the specific treatment.
In older children and adolescents evidence-based practice and knowledge has been well established while in neonates, infants and younger children due to the limited clinical experience and existing literature the approach must suggest a more prudence and great caution in order to improve patient safety and reduce side effects. In children below 2-3 years of age, more large studies are necessary to overcome the limits of 'adapting' to them the treatment from the experience gained in older children and adults[35-37].
Conflict of interest statementThe author has no competing interests to disclose. The author acknowledges that no specific funding source has been used for this paper.
The following is the Chinese translation of this paper, translated by Dr. MA Xiao-Lu (Department of Neonatology, Children's Hospital, Zhejiang University School Medicine).以下是本文的中文摘译。
通过选择性支气管插管进行单肺通气或孤立肺通气技术在儿科的应用
重症监护、全麻或术后的儿科患者是有可能需要进行单肺通气(one-lung ventilation)或孤立肺通气(independent-lung ventilation)的。该技术在儿科, 特别是6~8岁以下患儿中的应用最主要困难是缺乏合适的双腔导管(double-lumen tube)。支气管封堵器(bronchial blocker)或常规单腔管都被尝试用来给婴儿或幼童进行选择性支气管插管(selective bronchial intubation)和单肺通气。封堵器和单腔导管的主要缺陷是无法完全密封, 需要中断通气的这侧肺不容易萎陷和再次复张, 治疗过程中容易异位, 常需要纤维支气管镜来引导操作。
随着视频辅助胸腔镜手术的发展, 对儿童全麻下的机械通气技术有了更灵活的要求, 为了更好地开展手术, 选择性支气管插管、单肺通气技术的应用也逐渐增加。但市面上缺乏应用于新生儿、小婴儿和幼童的合适的导管依然是最大的问题。
孤立肺通气技术用于单侧肺部疾病的治疗最早始于二十世纪80年代后期, 此后也逐渐应用于心胸外科术后的患者。孤立肺通气对于预防术后肺部并发症具有重要作用。限制孤立肺通气技术在儿科重症监护中应用的最主要原因是缺乏儿科不同年龄段适用的双腔导管以及该技术操作的复杂性。"Marraro儿科支气管内双腔管"(mPEBT)的发明给儿科麻醉和重症监护领域带来了希望, 因为该导管可用于新生儿至4~5岁的儿童。
1 选择性支气管插管选择性支气管插管可以将导管选择性插入一侧主支气管, 实现单肺通气。青春期患者和年龄超过6~8岁的儿童可以通过成人的双腔导管来实现选择性支气管插管。由于缺乏合适的双腔导管, 新生儿和幼童的选择性支气管插管只能通过支气管封堵器配合单腔管实现, 而且只能单肺通气。
1.1 单肺通气单肺通气指仅用一侧肺通气, 让对侧肺处于萎陷状态。该技术常用于全麻下行心胸手术时, 因为一侧肺萎陷后更利于手术操作。气管-支气管瘘、严重气胸若经过胸腔引流不能改善可以尝试单肺通气。另外, 若病变(如出血、感染)仅累及一侧, 希望病变继续局限避免扩散至对侧时也可以采用单肺通气。
当一侧肺完全萎陷且灌注也中断时, 患者能够很好地耐受单肺通气。如果肺的通气和灌注都没有完全中断, 则患者可能发生低氧和二氧化碳潴留。
1.2 孤立肺通气孤立肺通气可以使一侧肺独立进行通气, 也可以使双侧肺分别进行通气, 分别应用不同的通气模式、潮气量、呼气末正压(PEEP)。孤立肺通气必须应用双腔导管或两根分别放置于气管和一侧主支气管的单腔导管才能实现。虽然左、右主支气管都可以进行选择性插管, 但最好还是行左侧的选择性插管, 因为右侧的选择性插管容易造成右上肺叶通气受阻后发生不张。
孤立肺通气的指征包括单侧肺部病变、双侧病变合并单侧肺不张、气胸、气管-支气管瘘、一侧感染或出血需要避免病变扩散至对侧等。术中可以通过孤立肺通气使一侧肺萎陷以便于手术操作, 术后可以通过孤立肺通气使萎陷的肺再次复张。孤立肺通气还可用于支气管-肺泡灌洗、选择性表面活性物质给药和其他药物局部给药。
2 选择性支气管插管的方法 2.1 双腔支气管导管通过插入双腔支气管导管可以对两侧肺分别用不同的模式和PEEP进行通气, 或阻断一侧肺的通气使其萎陷, 避免一侧肺的感染或出血扩散至对侧。超过6~8岁的患儿可以用类似于图 1成人用的双腔管来进行选择性支气管插管。
成人的双腔导管分为左侧和右侧两种, 原则上, 两种应该一样安全和有效, 但实际上右侧双腔导管容易导致右上肺不张, 因此其应用是有争议的。对于不同患儿年龄该选择何种型号的双腔导管, 并没有简单的判断标准, 目前认为最好的方法是测量胸部平片上气管的宽度。
双腔导管可以在直接喉镜和/或纤维喉镜下操作。20世纪90年代早期, 随着mPEBT的发明, 新生儿和4~5岁以下的幼童也能够进行选择性支气管插管和同步孤立肺通气, 但mPEBT目前还属于特殊产品, 并没有上市。
mPEBT由两根长短不同的不带囊的导管组合而成, 材料为医用级聚氯乙烯, 整个管壁上都有一条不透X线的蓝线可用于定位(图 2和图 3)。有不同型号的mPEBT分别用于新生儿、婴儿和4~5岁以下的儿童。mPEBT插入气道后, 是以图 5的方向穿过声带的, 因此组成mPEBT的两根导管上下组合在一起, 其所占的空间可以超过单腔管(图 4为内径3 mm的单腔管穿过声带, 图 5为内径3 mm和2.5 mm两根导管组合成的mPEBT穿过声带)。
插入mPEBT的操作可在直接喉镜下完成, 通常不需要纤维喉镜。由于导管不带囊, 可能会出现漏气, 使PEEP的水平变得不稳定。评估选择性支气管插管导管位置的方法有几种, 包括肺部听诊、选择性呼出气CO2监测、纤维镜检、胸片。
2.2 支气管封堵器支气管封堵器可直接放入气道内, 也可沿着常规气管导管放置。有不同类型的支气管封堵器, 可用于选择性支气管插管, 也可用于没有双腔导管或双腔导管无法置入时。支气管封堵器主要分为以下两类。
第一类:包括血栓取出术、动脉切开术、心导管术中所用的导管。这些导管都是"超适应证"应用的, 因为设计的初衷是为了其他的临床目的。但由于不同年龄的儿科患者缺乏相应的双腔导管, 这些支气管封堵器就成了选择之一。这些导管的远端带有可充气的球囊, 应注意球囊充气后产生的压力可能导致支气管黏膜缺血。用于动脉切开术的导管前端带有特殊角度, 更容易成功插入支气管, 是临床应用最多的导管。需注意的是, 如果这些封堵器是从常规气管导管置入的, 则会增加气管内的气流阻力, 导致通气困难。封堵器的正确位置可以通过双侧听诊来确定, 有条件进行纤维支气管镜检则更好。
第二类:把封堵器和气管导管合并成一体或将封堵器放入气管导管壁上的隧道内, 封堵器前端带有高容量、低压力的球囊。这一类封堵器需要在纤维支气管镜的引导下置入正确的位置。
导丝引导的Arndt封堵器®、UniventTM管、UniblockerTM可用于较大患儿的选择性支气管插管。Cohen®弹性尖端的支气管封堵器, CoopdechTM支气管封堵器, EZ-blockerTM、PapworthBiVent气管导管可用于成人, 但不能用于儿童。
导丝引导的Arndt封堵器®的中央是个空腔, 可以插入导丝, 导丝尖端是个环形, 能够固定住封堵器将其置入一侧主支气管。这一种封堵器有3种型号: 5 Fr、7 Fr和9 Fr。9 Fr可用于7.5 mm及更粗的气管导管; 7 Fr用于6.0~7.0 mm的气管导管; 5 Fr用于4.5~5.5 mm的气管导管。
UniventTM导管是标准的单腔气管导管, 分带囊和不带囊两种, 导管内有个单独的腔可以插入封堵器, 调整封堵器的位置, 使其到达支气管内。和整个导管的外径比起来, 气管导管的内径就比较小, 这就增加了气流的阻力。UniventTM管若内径是3.5 mm, 其外径就要7.5~8.0 mm, 因此无法用于幼儿。图 6是用于8~10岁以上患儿的UniventTM管, 分别为带囊和不带囊两种。UniventTM管中央有一个通道, 可以进行支气管吸引或送入氧气。当不需要孤立肺通气时, 可以把封堵器从气管导管内撤出, 保留的气管导管可继续进行常规通气。UniventTM管的放置需要技术熟练的操作者在纤维喉镜的引导下完成。
所有类型封堵器最常见的并发症是选择性支气管插管失败、封堵器在支气管内发生移位、球囊嵌入近端导管内、由于解剖结构异常无法实现孤立肺通气、球囊意外破裂。这些并发症如果没有及时发现和处理可导致严重的低氧血症。出了问题的封堵器要重新放置难度很大, 通常需要纤维支气管镜引导。
2.3 单腔支气管导管早在20世纪30年代就有尝试用普通的或经过改良的单腔气管导管进行支气管插管和孤立性肺通气。该技术利用常规气管导管或特殊的带囊/不带囊气管导管, 至今仍用于新生儿和婴儿。在没有合适的双腔导管或支气管封堵器时, 单腔支气管导管因具有足够的长度而被拿来试用。改良后的气管导管内径有4.0、5.0和6.0 mm 3种, 在所有儿童患者中, 当常规气管导管长度不够时都可以尝试用改良后的气管导管进行选择性支气管插管。
用常规气管导管进行选择性支气管插管时一般将患儿置于半侧卧位, 使支气管的解剖位置更利于置管, 还可能需要纤维支气管镜的引导。把合适的气管导管插入气管后, 逐步推进至左侧或右侧主支气管。通过听诊来判断导管置入的位置是否正确, 仅通气侧肺部可闻及呼吸音。如果选用的是不带囊的导管, 则很难达到支气管的完全密闭。必要时气管导管很容易从支气管撤退至气管, 这样很快就能恢复双侧肺部同时通气的状态。
临床上, 对于新生儿和小婴儿也可以插入两根常规的气管导管来进行选择性支气管插管和孤立肺通气。一根气管导管插入一侧主支气管, 实现选择性支气管插管, 另一根插入气管对对侧肺进行通气, 如图 7和图 8所示。通常, 经鼻插管更容易固定, 能减少脱管的风险。如果没有双腔导管而患儿又确实需要孤立肺通气时可以试用该方法。
不同支气管导管的优缺点和应用局限性见表 2。
| 表 2 不同支气管导管的优缺点和应用局限性 |
|
|
如果通气非常困难, 可能需要重新放置气管导管、双腔导管和/或支气管封堵器, 需要把原有装置移除, 用面罩皮囊通气, 等氧合恢复正常后才能再次进行插管操作。单肺通气过程中, 严重的气道损伤如皮下气肿、炎症、机械损伤、获得性支气管狭窄很少发生。气胸和其他气漏、气道出血、气管导管或支气管导管的球囊突出进入手术部位是很罕见的并发症。一旦发生这些并发症, 应立即行支气管镜检查, 并给予合适的治疗。
3 关于改善安全性和降低并发症的思考目前对于NICU、PICU、麻醉、手术的患儿, 大家越来越关注治疗的安全性及质量。在应用新的生物制剂、新的仪器设备时, 若没有经过充分的实验论证, 就会出现潜在的风险和并发症, 甚至带来医学-法律问题。选择性支气管插管是一个很重要的技术, 重症监护、全麻、术中和术后护理的患儿都有可能需要。
婴儿和幼年患儿实施选择性支气管插管的所有方法都是复杂的, 需要很高的知识和技能的要求, 必须避免在没有充分准备的情况下实施选择性支气管插管。在治疗全程中应结合儿科患者的解剖和生理特点全面评估选择性支气管插管的优点、缺点、局限性, 以及各种不同的设备, 并评估治疗小组中医护人员的相关经验。
在较大儿童或青春期患者, 这些技术已经有了比较好的循证基础, 但在新生儿、小婴儿和幼童, 临床经验较为欠缺, 发表的文献也较少, 因此需要更加谨慎, 尽量避免并发症, 增加安全性。
(翻译:马晓路, 浙江大学医学院附属儿童医院NICU)
| [1] |
Byon HJ, Lee JW, Kim JK, et al. Anesthetic management of video-assisted thoracoscopic surgery (VATS) in pediatric patients:the issue of safety in infant and younger children[J]. Korean J Anesthesiol, 2010, 59(2): 99-103. DOI:10.4097/kjae.2010.59.2.99 (  0) 0) |
| [2] |
Carlon GC, Kahn R, Howland WS, et al. Acute life-threatening ventilation-perfusion inequality:an indication for independent lung ventilation[J]. Crit Care Med, 1978, 6(6): 380-383. DOI:10.1097/00003246-197811000-00009 (  0) 0) |
| [3] |
Marraro G. Simultaneous independent lung ventilation in pediatric patients[J]. Crit Care Clin, 1992, 8(1): 131-145. DOI:10.1016/S0749-0704(18)30271-9 (  0) 0) |
| [4] |
Marraro G. Selective endobronchial intubation in paediatrics:the Marraro Paediatric Bilumen Tube[J]. Paediatr Anaesth, 1994, 4(4): 255-258. DOI:10.1111/j.1460-9592.1994.tb00174.x (  0) 0) |
| [5] |
Pawar DK, Marraro GA. One lung ventilation in infants and children:experience with Marraro double lumen tube[J]. Paediatr Anaesth, 2005, 15(3): 204-208. DOI:10.1111/j.1460-9592.2005.01421.x (  0) 0) |
| [6] |
Licker M, Le Guen M, Diaper J, et al. Isolation of the lung:double-lumen tubes and endobronchial blockers[J]. Trends Anaesth Crit Care, 2014, 4(2/3): 47-54. (  0) 0) |
| [7] |
Huo JM, Bai K, Fu YQ, et al. Clinical efficacy of one-lung ventilation in treatment of children postoperatively intractable atelectasis[J]. Zhonghua Er Ke Za Zhi, 2017, 55(11): 840-843. (  0) 0) |
| [8] |
Hammer GB. Pediatric thoracic anesthesia[J]. Anesthesiol Clin North Am, 2002, 20(1): 153-180. DOI:10.1016/S0889-8537(03)00059-2 (  0) 0) |
| [9] |
Marraro G. Airway management[M]//Bissonnette B. Pediatric Anesthesia. Shelton: People's Medical Publishing House, 2011: 1167-1185.
(  0) 0) |
| [10] |
Fabila TS, Menghraj SJ. One lung ventilation strategies for infants and children undergoing video assisted thoracoscopic surgery[J]. Indian J Anaesth, 2013, 57(4): 339-344. DOI:10.4103/0019-5049.118539 (  0) 0) |
| [11] |
Templeton TW, Downard MG, Simpson CR, et al. Bending the rules:a novel approach to placement and retrospective experience with the 5 French Arndt endobronchial blocker in children <2 years[J]. Paediatr Anaesth, 2016, 26(5): 512-520. DOI:10.1111/pan.12882 (  0) 0) |
| [12] |
Ehrenfeld JM, Mulvoy W, Sandberg WS. Performance comparison of right- and left-sided double-lumen tubes among infrequent users[J]. J Cardiothorac Vasc Anesth, 2010, 24(4): 598-601. DOI:10.1053/j.jvca.2009.09.007 (  0) 0) |
| [13] |
Kaplan T, Ekmekçi P, Kazbek BK, et al. Endobronchial intubation in thoracic surgery:which side should be preferred?[J]. Asian Cardiovasc Thorac Ann, 2015, 23(7): 842-845. DOI:10.1177/0218492315591105 (  0) 0) |
| [14] |
Brodsky JB, Lemmens HJ. Tracheal width and left double-lumen tube size:a formula to estimate left-bronchial width[J]. J Clin Anesth, 2005, 17(4): 267-270. DOI:10.1016/j.jclinane.2004.07.008 (  0) 0) |
| [15] |
Marraro G. Synchronized independent lung ventilation in pediatric age[J]. Appl Cardiopulm Pathophysiol, 1987, 2(1): 283-288. (  0) 0) |
| [16] |
de Bellis M, Accardo R, Di Maio M, et al. Is flexible bronchoscopy necessary to confirm the position of double-lumen tubes before thoracic surgery?[J]. Eur J Cardiothorac Surg, 2011, 40(4): 912-916. DOI:10.1016/j.ejcts.2011.01.070 (  0) 0) |
| [17] |
Bhirud PH, Toal PV. A different fibre-optic device for double lumen tube position confirmation![J]. Indian J Anaesth, 2016, 60(4): 298-300. DOI:10.4103/0019-5049.179476 (  0) 0) |
| [18] |
Das SK, Choupoo NS, Haldar R, et al. Transtracheal ultrasound for verification of endotracheal tube placement:a systematic review and meta-analysis[J]. Can J Anaesth, 2015, 62(4): 413-423. DOI:10.1007/s12630-014-0301-z (  0) 0) |
| [19] |
Parab SY, Divatia JV, Chogle A. A prospective comparative study to evaluate the utility of lung ultrasonography to improve the accuracy of traditional clinical methods to confirm position of left sided double lumen tube in elective thoracic surgeries[J]. Indian J Anaesth, 2015, 59(8): 476-481. DOI:10.4103/0019-5049.162983 (  0) 0) |
| [20] |
Letal M, Theam M. Paediatric lung isolation[J]. BJA Educ, 2017, 17(2): 57-62. DOI:10.1093/bjaed/mkw047 (  0) 0) |
| [21] |
Neustein SM. Pro:bronchial blockers should be used routinely for providing one-lung ventilation[J]. J Cardiothorac Vasc Anesth, 2015, 29(1): 234-236. DOI:10.1053/j.jvca.2014.07.028 (  0) 0) |
| [22] |
Brodsky JB. Con:a bronchial blocker is not a substitute for a double-lumen endobronchial tube[J]. J Cardiothorac Vasc Anesth, 2015, 29(1): 237-239. DOI:10.1053/j.jvca.2014.07.027 (  0) 0) |
| [23] |
Kamra SK, Jaiswal AA, Garg AK, et al. Rigid bronchoscopic placement of fogarty catheter as abronchial blocker for one lung isolation and ventilation in infants and children undergoing thoracic surgery:a single institution experience of 27 cases[J]. Indian J Otolaryngol Head Neck Surg, 2017, 69(2): 159-171. DOI:10.1007/s12070-016-1026-9 (  0) 0) |
| [24] |
Garg R. Airway management techniques for one lung ventilation in children-what else![J]. Indian J Anaesth, 2014, 58(1): 100-101. DOI:10.4103/0019-5049.126855 (  0) 0) |
| [25] |
Kus A, Hosten T, Gurkan Y, et al. A comparison of the EZ-blocker with a cohen flex-tip blocker for one-lung ventilation[J]. J Cardiothorac Vasc Anesth, 2014, 28(4): 896-899. DOI:10.1053/j.jvca.2013.02.006 (  0) 0) |
| [26] |
Ozaki M, Murashima K, Koga K, et al. Use of the coopdech bronchial blocker as a tracheal tube introducer in a patient with difficult laryngoscopy[J]. J Anesth, 2010, 24(2): 319-320. DOI:10.1007/s00540-010-0890-9 (  0) 0) |
| [27] |
Templeton TW, Templeton LB, Lawrence AE, et al. An initial experience with an Extraluminal EZ-Blocker®:a new alternative for 1-lung ventilation in pediatric patients[J]. Paediatr Anaesth, 2018, 28(4): 347-351. DOI:10.1111/pan.13342 (  0) 0) |
| [28] |
Weng H, Xu ZY, Liu J, et al. Placement of the univent tube without fiberoptic bronchoscope assistance[J]. Anesth Analg, 2010, 110(2): 508-514. DOI:10.1213/ANE.0b013e3181c5ed18 (  0) 0) |
| [29] |
Wigginton M, Lehrian L. Alternative methods of lung isolation in cases of pediatric bilateral thoracoscopic surgery[J]. Paediatr Anaesth, 2016, 26(12): 1209-1211. DOI:10.1111/pan.13012 (  0) 0) |
| [30] |
Theroux MC, Fisher AO, Rodriguez ME, et al. Prophylactic methylprednisolone to reduce inflammation and improve outcomes from one lung ventilation in children:a randomized clinical trial[J]. Paediatr Anaesth, 2015, 25(6): 587-594. DOI:10.1111/pan.12601 (  0) 0) |
| [31] |
Goussard P, Morrison J, Bekker A, et al. Acquired neonatal bronchial stenosis after selective intubation:successful managed with balloon dilatation[J]. Clin Case Rep, 2019, 7(5): 917-919. DOI:10.1002/ccr3.2112 (  0) 0) |
| [32] |
Samuels-Reid J, Cope JU, Morrison AE. Device safety and effectiveness in the pediatric population:a US FDA perspective[J]. Expert Rev Med Devices, 2009, 6(2): 131-135. DOI:10.1586/17434440.6.2.131 (  0) 0) |
| [33] |
Pascall E, Trehane SJ, Georgiou A, et al. Litigation associated withintensive care unit treatment in England:an analysis of NHSLA data1995-2012[J]. Br J Anaesth, 2015, 115(4): 601-607. DOI:10.1093/bja/aev285 (  0) 0) |
| [34] |
Marraro GA, Yu R, Liang Y, et al. Best clinical practice and evidence-based assessment in pediatric ventilation support[J]. Pediatr Crit Care Med, 2016, 17(11): 1097-1099. DOI:10.1097/PCC.0000000000000963 (  0) 0) |
| [35] |
Marraro GA, Spada C. Simulation as a learning tool for pediatric anesthetists[J]. World Clin Anesth Crit Care Pain, 2014, 2(2): 322-342. (  0) 0) |
| [36] |
Failor E, Bowdle A, Jelacic S, et al. High-fidelity simulation of lung isolation with double-lumen endotracheal tubes and bronchial blockers in anesthesiology resident training[J]. J Cardiothorac Vasc Anesth, 2014, 28(4): 865-869. DOI:10.1053/j.jvca.2013.07.015 (  0) 0) |
| [37] |
Ambardekar AP, Black S, Singh D, et al. The impact of simulation-based medical education on resident management of emergencies in pediatric anesthesiology[J]. Paediatr Anaesth, 2019, 29(7): 753-759. DOI:10.1111/pan.13652 (  0) 0) |
 2020, Vol. 22
2020, Vol. 22

