 PDF(529 KB)
PDF(529 KB)


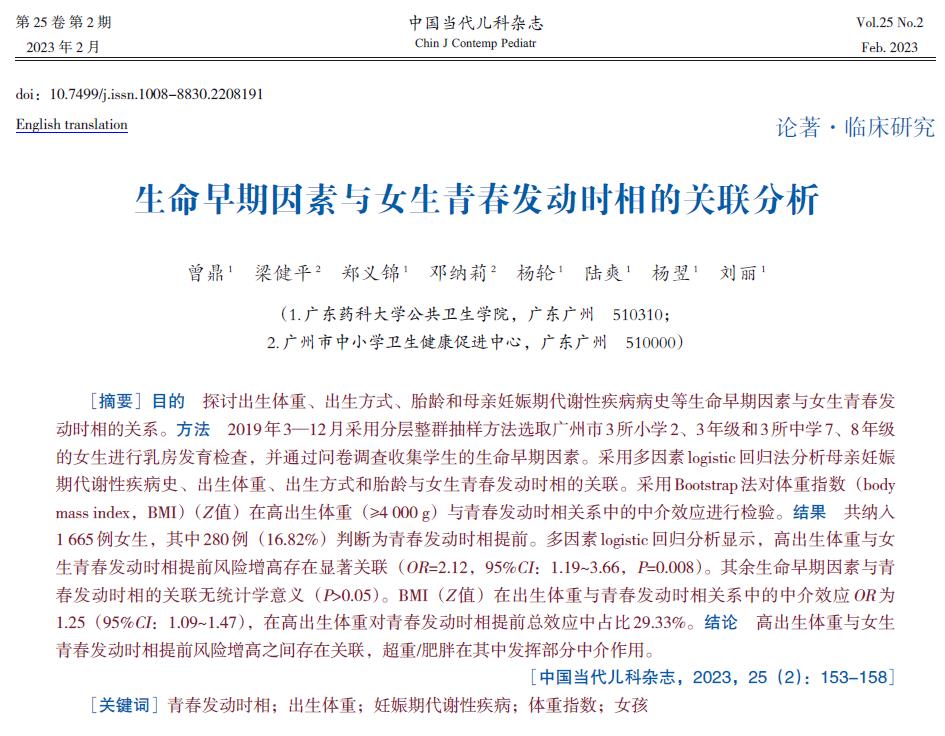
Association between early-life factors and pubertal timing in girls
ZENG Ding, LIANG Jian-Ping, ZHENG Yi-Jin, DENG Na-Li, YANG Lun, LU Shuang, YANG Yi, LIU Li
Chinese Journal of Contemporary Pediatrics ›› 2023, Vol. 25 ›› Issue (2) : 153-158.
 PDF(529 KB)
PDF(529 KB)
 PDF(529 KB)
PDF(529 KB)
Association between early-life factors and pubertal timing in girls
Pubertal timing / Birth weight / Gestational metabolic disorder / Body mass index / Girl