 PDF(576 KB)
PDF(576 KB)


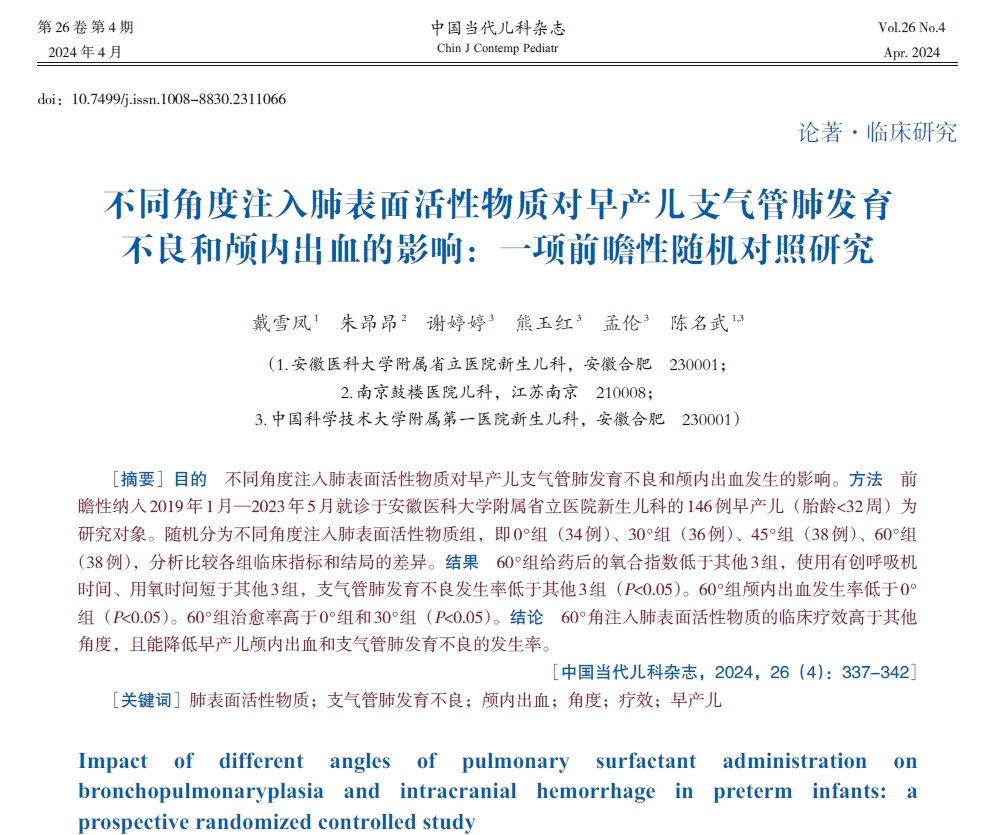
Impact of different angles of pulmonary surfactant administration on bronchopulmonaryplasia and intracranial hemorrhage in preterm infants: a prospective randomized controlled study
DAI Xue-Feng, ZHU Ang-Ang, XIE Ting-Ting, XIONG Yu-Hong, MENG Lun, CHEN Ming-Wu
Chinese Journal of Contemporary Pediatrics ›› 2024, Vol. 26 ›› Issue (4) : 337-342.
 PDF(576 KB)
PDF(576 KB)
 PDF(576 KB)
PDF(576 KB)
Impact of different angles of pulmonary surfactant administration on bronchopulmonaryplasia and intracranial hemorrhage in preterm infants: a prospective randomized controlled study
Pulmonary surfactant / Bronchopulmonary dysplasia / Intracranial hemorrhage / Angle / Efficacy / Preterm infant