 PDF(821 KB)
PDF(821 KB)


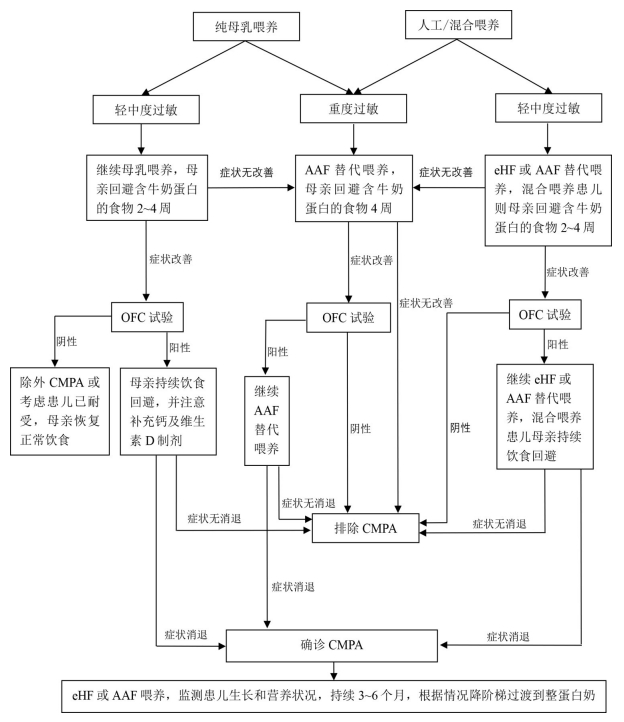
Interpretation of key points from the "Expert Consensus on Diagnosis and Management of Neonatal Cow Milk Protein Allergy (2023)"
ZHANG Xin-Yin, LIU Li-Ting, BAO Lei, SHI Yuan
Chinese Journal of Contemporary Pediatrics ›› 2024, Vol. 26 ›› Issue (11) : 1127-1134.
 PDF(821 KB)
PDF(821 KB)
 PDF(821 KB)
PDF(821 KB)
Interpretation of key points from the "Expert Consensus on Diagnosis and Management of Neonatal Cow Milk Protein Allergy (2023)"
Cow's milk protein allergy / Dietary management / Nutritional management / Neonate