 PDF(1172 KB)
PDF(1172 KB)


Effect of hypothermia therapy on serum GFAP and UCH-L1 levels in neonates with hypoxic-ischemic encephalopathy
JIANG Shu-Hong, WANG Jin-Xiu, ZHANG Yi-Ming, JIANG Hui-Fen
Chinese Journal of Contemporary Pediatrics ›› 2014, Vol. 16 ›› Issue (12) : 1193-1196.
 PDF(1172 KB)
PDF(1172 KB)
 PDF(1172 KB)
PDF(1172 KB)
Effect of hypothermia therapy on serum GFAP and UCH-L1 levels in neonates with hypoxic-ischemic encephalopathy
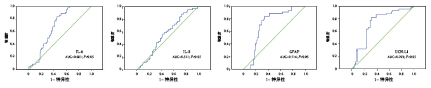
Objective To evaluate the effect of hypothermia therapy on serum glial fibrillary acidic protein (GFAP) and ubiquitin carboxyl-terminal hydrolase L1 (UCH-L1) levels in neonates with hypoxic-ischemic encephalopathy (HIE). Methods Sixty-four HIE neonates were enrolled in this study. Thirty-three neonates with mild HIE were given conventional treatment and 31 neonates with moderate or severe HIE received conventional treatment and hypothermia therapy. Serum levels of GFAP and UCH-L1 were measured using ELISA before treatment and 6-12 hours after treatment. Results Serum levels of IL-6, IL-8, GFAP and UCH-L1 in the moderate/severe HIE group were significantly higher than in the mild HIE group (P<0.05) before treatment. Serum GFAP level was positively correlated with serum IL-6 (r=0.54; P<0.05) and IL-8 levels (r=0.63; P<0.05) , while negatively correlated with Apgar score (r=-0.47, P<0.05). After treatment, serum levels of IL-6, IL-8 and UCH-L1 in the moderate/severe HIE group were significantly reduced (P<0.05), while serum GFAP levels increased significantly (P<0.05). The patients with abnormal neurological development showed higher serum GFAP levels than those with favourable prognosis (P<0.05). Receiver operating characteristic (ROC) curves analysis demonstrated that the area under curve (AUC) of GFAP and UCH-L1 were 0.714 and 0.703 respectively. At a cut-off value of 0.07 ng/mL, the sensitivity and specificity of GFAP for the diagnosis of HIE were 77% and 78% respectively. Conclusions Hypothermia therapy can decrease serum UCH-L1 levels and increase serum GFAP levels in neonates with HIE. Based on their diagnostic value of brain injury, GFAP and UCH-L1 are promising to be novel biomarkers for HIE.
Hypoxic-ischemic encephalopathy / Hypothermia therapy Glial fibrillary acidic protein / Ubiquitin carboxyl-terminal hydrolase L1 / Neonate