PDF(1016 KB)
PDF(1016 KB)


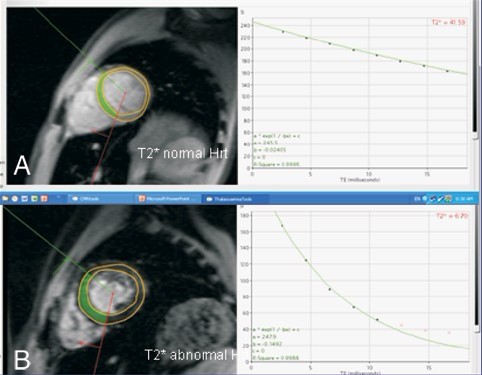
Evaluation of heart and liver iron deposition status in patients with β- thalassemia intermedia and major with MRI T2* technique
LI Chang-Gang, LIU Si-Xi, MAI Hui-Rong, WANG Ying, WEN Fei-Qiu, LIU Ri-Yang, ZHANG Xin-Hua, Winnie Chiu Wing CHU, AU Wing-Yan
Chinese Journal of Contemporary Pediatrics ›› 2012, Vol. 14 ›› Issue (2) : 110-113.
 PDF(1016 KB)
PDF(1016 KB)
 PDF(1016 KB)
PDF(1016 KB)
Evaluation of heart and liver iron deposition status in patients with β- thalassemia intermedia and major with MRI T2* technique