 PDF(1336 KB)
PDF(1336 KB)


Clinical features of children with SARS-CoV-2 infection: an analysis of 13 cases from Changsha, China
TAN Xin, HUANG Juan, ZHAO Fen, ZHOU Yan, LI Jie-Qiong, WANG Xiang-Yun
Chinese Journal of Contemporary Pediatrics ›› 2020, Vol. 22 ›› Issue (4) : 294-298.
 PDF(1336 KB)
PDF(1336 KB)
 PDF(1336 KB)
PDF(1336 KB)
Clinical features of children with SARS-CoV-2 infection: an analysis of 13 cases from Changsha, China
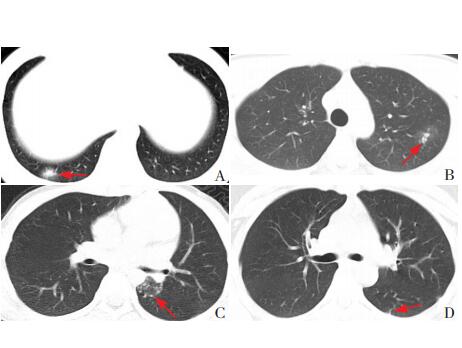
Objective To study the clinical features of children with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Methods A retrospective analysis was performed for the clinical data of 13 children with SARS-CoV-2 infection who hospitalized in a Changsha hospital. Results All 13 children had the disease onset due to family aggregation. Of the 13 children, 2 had no symptoms, and the other 11 children had the clinical manifestations of fever, cough, pharyngeal discomfort, abdominal pain, diarrhea, convulsions, or vomiting. As for clinical typing, 7 had mild type, 5 had common type, and 1 had severe type. The median duration of fever was 2 days in 6 children. All 13 children had normal levels of peripheral blood lymphocyte counts, immunoglobulins, CD4, CD8, and interleukin-6. The median time to clearance of SARS-CoV-2 was 13 days in the nasopharyngeal swabs of the 13 children. Three children presented false negatives for RT-PCR of SARS-CoV-2. SARS-CoV-2 RNA remained detectable in stools for 12 days after the nasopharyngeal swab test yielded a negative result. Abnormal CT findings were observed in 6 children. All 13 children were cured and discharged and they were normal at 2 weeks after discharge. Conclusions Intra-family contact is the main transmission route of SARS-CoV-2 infection in children, and there is also a possibility of fecal-oral transmission. Mild and common types are the major clinical types in children with SARS-CoV-2 infection, and cytokine storm is not observed. Children with SARS-CoV-2 infection tend to have a good short-term prognosis, and follow-up is needed to observe their long-term prognosis. Multiple nucleic acid tests should be performed for patients with SARS-CoV-2 infection and their close contacts by multiple site sampling.
[1] Gorbalenya AE, Baker SC, Baric RS, et al. Severe acute respiratory syndrome-related coronavirus:the species and its viruses-a statement of the Coronavirus Study Group[J/OL].Biorxiv. (2020-02-11)[2020-03-22]. https://www.biorxiv.org/content/10.1101/2020.02.07.937862v1.
[2] Chan JF, Kok KH, Zhu Z, et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan[J]. Emerg Microbes Infect, 2020, 9(1):221-236.
[3] 中华人民共和国国家卫生健康委员会. 截至3月23日24时新型冠状病毒肺炎疫情最新情况[EB/OL]. (2020-03-24)[2020-03-24]. http://www.nhc.gov.cn/xcs/yqtb/202003/e6c12d0c2cf04474944187f4088dc021.shtml.
[4] 国家卫生健康委办公厅, 国家中医药管理局办公室. 新型冠状病毒肺炎诊疗方案(试行第六版)[EB/OL]. (2020-02-18)[2020-03-22]. http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2.shtml.
[5] 陈志敏, 傅君芬, 舒强, 等. 儿童2019冠状病毒病(COVID-19)诊疗指南(第二版)[J]. 浙江大学学报(医学版), 2020. DOI:10.3785/j.issn.1008-9292.2020.02.01. 网络预发表.
[6] Sun K, Chen J, Viboud C. Early epidemiological analysis of the coronavirus disease 2019 outbreak based on crowdsourced data:a population-level observational study[J/OL]. Lancet Digit Health. (2020-02-20)[2020-03-22]. http://www.chengjipharm.com/uploads/file1/20200221/5e4fa89b6fbe8.pdf.
[7] Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating personto-person transmission:a study of a family cluster[J]. Lancet, 2020, 395(10223):514-523.
[8] 蔡洁皓, 王相诗, 葛艳玲, 等. 上海首例儿童新型冠状病毒感染[J]. 中华儿科杂志, 2020, 58(2):86-87.
[9] Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan China[J]. Lancet, 2020, 395(10223):497-506.
[10] Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome[J/OL]. Lancet Respir Med. (2020-02-17)[2020-03-30]. https://www.thelancet.com/action/showPdf?pii=S2213-2600%2820%2930076-X.
[11] 王劲, 王丹, 陈国策, 等. 以消化道症状为首发表现的新生儿SARS-CoV-2感染1例[J]. 中国当代儿科杂志, 22(3):211-214.
[12] 冯凯, 云永兴, 王险峰, 等. 儿童新型冠状病毒感染15例CT影像特征分析[J]. 中华儿科杂志, 2020. DOI:10.3760/cma. j.issn.0578-1310.2020.0007. 网络预发表.
[13] Channappanavar R, Perlman S. Pathogenic human coronavirus infections:causes and consequences of cytokine storm and immunopathology[J]. Semin Immunopathol, 2017, 39(5):529-539.