PDF(556 KB)
PDF(556 KB)


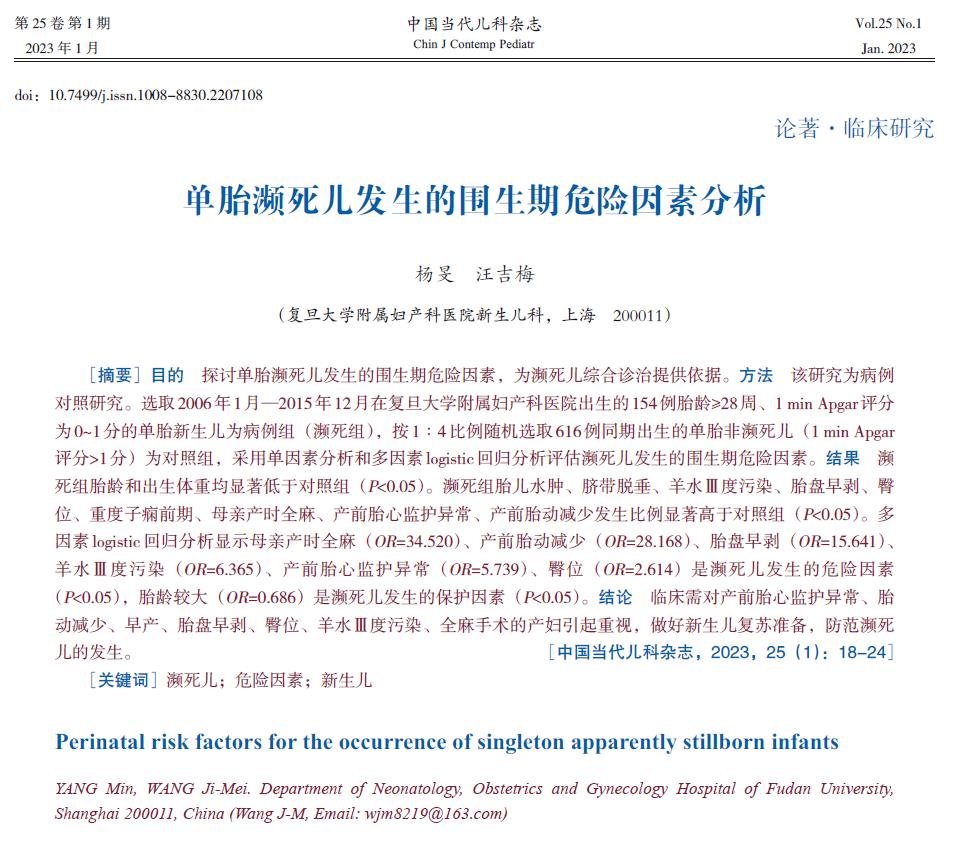
Perinatal risk factors for the occurrence of singleton apparently stillborn infants
YANG Min, WANG Ji-Mei
Chinese Journal of Contemporary Pediatrics ›› 2023, Vol. 25 ›› Issue (1) : 18-24.
 PDF(556 KB)
PDF(556 KB)
 PDF(556 KB)
PDF(556 KB)
Perinatal risk factors for the occurrence of singleton apparently stillborn infants