 PDF(1973 KB)
PDF(1973 KB)


微绒毛包涵体病一家系临床特点和MYO5B基因突变分析
程映, 梁红, 蔡娜莉, 郭丽, 黄宇戈, 宋元宗
中国当代儿科杂志 ›› 2017, Vol. 19 ›› Issue (9) : 968-974.
 PDF(1973 KB)
PDF(1973 KB)
 PDF(1973 KB)
PDF(1973 KB)
微绒毛包涵体病一家系临床特点和MYO5B基因突变分析
Clinical features and MYO5B mutations of a family affected by microvillus inclusion disease
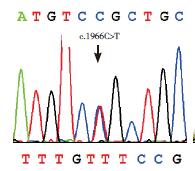
微绒毛包涵体病(MVID)是MYO5B或STX3基因突变导致的一种常染色体隐性遗传病,以难治性腹泻和营养吸收障碍为主要临床表现。本文探讨1例MVID患儿的临床特征及MYO5B基因突变特点。患儿为21 d女婴,因"解稀便20 d"收住院。体查发现患儿体重和身长落后,皮肤巩膜黄染;双肺呼吸音清,心音有力;腹部膨隆,腹壁静脉显露,肝脾肋下未触及。血生化结果发现总胆汁酸、胆红素、转氨酶、谷氨酰转肽酶等指标均升高,而血钠、氯、磷和镁水平均降低。血气分析提示代谢性酸中毒。初步诊断先天性腹泻,给予肠外营养及对症支持治疗。患儿腹泻顽固,代谢性酸中毒和电解质絮乱难以纠正,且转氨酶、谷氨酰转肽酶、总胆汁酸、胆红素等胆汁淤积指标持续高于正常。住院1月余自动出院,出院后失访。遗传学分析在患儿MYO5B基因检测到c.1966C > T(p.R656C)和c.310+2Tdup两个突变,分别来源于其母亲和父亲;其中c.310+2Tdup为新的剪接位点突变,最终患儿确诊为MVID。
Microvillus inclusion disease (MVID) is an autosomal recessive disorder caused by biallelic mutations in the MYO5B or STX3 gene. Refractory diarrhea and malabsorption are the main clinical manifestations. The aim of this study was to investigate the clinical features and MYO5B gene mutations of an infant with MVID. A 21-day-old female infant was referred to the hospital with the complaint of diarrhea for 20 days. On physical examination, growth retardation of the body weight and length was found along with moderately jaundiced skin and sclera. Breath sounds were clear in the two lungs and the heart sounds were normal. The abdomen was distended and the veins in the abdominal wall were observed. The liver and spleen were not palpable. Biochemical analysis revealed raised serum total bile acids, bilirubin, transaminases and γ-glutamyl transpeptidase while decreased levels of serum sodium, chloride, phosphate and magnesium. Blood gas analysis indicated metabolic acidosis. The preliminary diagnosis was congenital diarrhea, and thus parenteral nutrition was given along with other symptomatic and supportive measures. However, diarrhea, metabolic acidosis and electrolyte disturbance were intractable, and the cholestatic indices, including transaminases, γ-glutamyl transpeptidase, bilirubin and total bile acids, remained at increased levels. One month later, the patient was discharged and then lost contact. On genetic analysis, the infant was proved to be a compound heterozygote of the c.310+2Tdup and c.1966C > T(p.R656C) variants of the gene MYO5B, with c.310+2Tdup being a novel splice-site mutation. MVID was thus definitely diagnosed.
微绒毛包涵体病 / MYO5B基因 / 腹泻 / 剪接位点突变 / 新生儿
Microvillus inclusion disease / MYO5B gene / Diarrhea / Splice-site mutation / Newborn infant
[1] Cutz E, Rhoads JM, Drumm B, et al. Microvillus inclusion disease:an inherited defect of brush-border assembly and differentiation[J]. N Engl J Med, 1989, 320(10):646-651.
[2] Ruemmele FM, Schmitz J, Goulet O. Microvillous inclusion disease (microvillous atrophy)[J]. Orphanet J Rare Dis, 2006, 1:22.
[3] Davidson GP, Cutz E, Hamilton JR, et al. Familial enteropathy:a syndrome of protracted diarrhea from birth, failure to thrive, and hypoplastic villus atrophy[J]. Gastroenterology, 1978, 75(5):783-790.
[4] van der Velde KJ, Dhekne HS, Swertz MA, et al. An overview and online registry of microvillus inclusion disease patients and their MYO5B mutations[J]. Hum Mutat, 2013, 34(12):1597-1605.
[5] Phillips AD, Schmitz J. Familial microvillous atrophy:a clinicopathological survey of 23 cases[J]. J Pediatr Gastroenterol Nutr, 1992, 14(4):380-396.
[6] Michaux G, Massey-Harroche D, Nicolle O, et al. The localisation of the apical Par/Cdc42 polarity module is specifically affected in microvillus inclusion disease[J]. Biol Cell, 2016, 108(1):19-28.
[7] Qiu YL, Gong JY, Feng JY, et al. Defects in myosin VB are associated with a spectrum of previously undiagnosed low γ-glutamyltransferase cholestasis[J]. Hepatology, 2017, 65(5):1655-1669.
[8] Chen Y, Tian L, Zhang F, et al. Myosin Vb gene is associated with schizophrenia in Chinese Han population[J]. Psychiatry Res, 2013, 207(1-2):13-18.
[9] 毛曼, 郭丽, 张占会, 等. 微绒毛包涵体病一家系的表型及遗传学分析[J]. 中华医学遗传学杂志, 2016, 33(6):792-796.
[10] Xue Y, Ankala A, Wilcox WR, et al. Solving the molecular diagnostic testing conundrum for Mendelian disorders in the era of next-generation sequencing:single-gene, gene panel, or exome/genome sequencing[J]. Genet Med, 2015, 17(6):444-451.
[11] Sun Y, Ruivenkamp CA, Hoffer MJ, et al. Next-generation diagnostics:gene panel, exome, or whole genome?[J]. Hum Mutat, 2015, 36(6):648-655.
[12] Müller T, Hess MW, Schiefermeier N, et al. MYO5B mutations cause microvillus inclusion disease and disrupt epithelial cell polarity[J]. Nat Genet, 2008, 40(10):1163-1165.
[13] Engevik AC, Goldenring JR. Trafficking ion transporters to the apical membrane of polarized intestinal enterocytes[J]. Cold Spring Harb Perspect Biol, 2017.[Epub ahead of print]
[14] Girard M, Lacaille F, Verkarre V, et al. MYO5B and bile salt export pump contribute to cholestatic liver disorder in microvillous inclusion disease[J]. Hepatology, 2014, 60(1):301-310.
[15] Siahanidou T, Koutsounaki E, Skiathitou AV, et al. Extraintestinal manifestations in an infant with microvillus inclusion disease:complications or features of the disease?[J]. Eur J Pediatr, 2013, 172(9):1271-1275.
[16] Gonzales E, Taylor SA, Davit-Spraul A, et al. MYO5B mutations cause cholestasis with normal serum gamma-glutamyl transferase activity in children without microvillous inclusion disease[J]. Hepatology, 2017, 65(1):164-173.
[17] Vogel GF, Janecke AR, Krainer IM, et al. Abnormal Rab11-Rab8-vesicles cluster in enterocytes of patients with microvillus inclusion disease[J]. Traffic, 2017, 18(7):453-464.
[18] Erickson RP, Larson-Thomé K, Valenzuela RK, et al. Navajo microvillous inclusion disease is due to a mutation in MYO5B[J]. Am J Med Genet A, 2008, 146A(24):3117-3119.
[19] Szperl AM, Golachowska MR, Bruinenberg M, et al. Functional characterization of mutations in the myosin Vb gene associated with microvillus inclusion disease[J]. J Pediatr Gastroenterol Nutr, 2011, 52(3):307-313.
[20] Ruemmele FM, Müller T, Schiefermeier N, et al. Loss-of-function of MYO5B is the main cause of microvillus inclusion disease:15 novel mutations and a CaCo-2 RNAi cell model[J]. Hum Mutat, 2010, 31(5):544-551.
[21] Kelly DA. Preventing parenteral nutrition liver disease[J]. Early Hum Dev, 2010, 86(11):683-687.
[22] Ruemmele FM, Jan D, Lacaille F, et al. New perspectives for children with microvillous inclusion disease:early small bowel transplantation[J]. Transplantation, 2004, 77(7):1024-1028.
[23] van Hoeve K, Hoffman I, Fusaro F, et al. Microvillus inclusion disease:a subtotal enterectomy as a bridge to transplantation[J]. Acta Chir Belg, 2016, 116(6):333-339.
国家自然科学基金(81570793)。