 PDF(1392 KB)
PDF(1392 KB)


 PDF(1392 KB)
PDF(1392 KB)
 PDF(1392 KB)
PDF(1392 KB)
γδ T细胞在儿童过敏性紫癜免疫微环境中的表达和意义
Expression of gamma-delta T cells in immune microenvironment in children with Henoch-Schönlein purpura
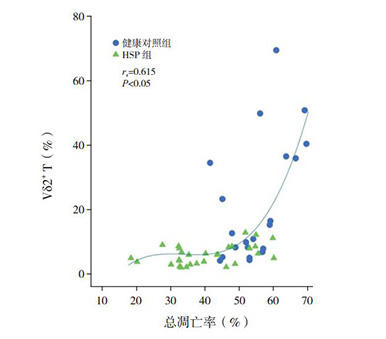
目的 探讨γδ T细胞及其细胞亚群在儿童过敏性紫癜(HSP)免疫发病机制中的作用,从调控γδ T细胞作为切入点,为儿童HSP的治疗提供新思路。方法 以33例HSP患儿(HSP组)和21例健康儿童(健康对照组)为研究对象,比较两组外周血单个核细胞(PBMCs)中γδ T及其细胞亚群Vδ1+T、Vδ2+T等表达水平、γδ T细胞凋亡率及IL-17水平。结果 HSP组PBMCs中淋巴细胞比例、γδ T细胞中Vδ2+T比例低于健康对照组(P < 0.05)。HSP组γδ T细胞中Vδ1+T比例、血浆IL-17水平高于健康对照组(P < 0.05)。HSP组γδ T细胞总凋亡率低于健康对照组(P < 0.05),其中以早期凋亡为著。Vδ2+T表达与γδ T细胞总凋亡率呈正相关(rs=0.615,P < 0.05),与IL-17水平呈负相关(rs=-0.398,P < 0.05)。结论 γδ T细胞介导的Vδ1+/Vδ2+T免疫失衡及IL-17炎症因子过度激活可能参与HSP的发生,其中Vδ2+T诱导的免疫耐受被打破可能是疾病发生的重要病理生理基础。
Objective To study the role of gamma-delta T (γδ T) cells and its subsets in the immunopathogenesis of Henoch-Schönlein purpura (HSP) in children, and to provide new ideas for the treatment of HSP in children from the aspect of γδ T cell regulation. Methods A total of 33 children with HSP were enrolled as the HSP group, and 21 healthy children were enrolled as the healthy control group. The percentages of γδ T cells and its subsets Vδ1+T and Vδ2+T cells among peripheral blood mononuclear cells (PBMCs) were measured, as well as the apoptosis rate of γδ T cell and plasma level of interleukin-17 (IL-17). Results Compared with the healthy control group, the HSP group had significantly lower percentages of lymphocytes in PBMCs and Vδ2+T cells in γδ T cells (P < 0.05). The HSP group had significantly higher percentage of Vδ1+T cells in γδ T cells and plasma level of IL-17 than the healthy control group. The HSP group had a significantly higher overall apoptosis rate of γδ T cells than the healthy control group (P < 0.05), especially early apoptosis. The percentage of Vδ2+T cells was positively correlated with overall apoptosis rate (rs=0.615, P < 0.05) and was negatively correlated with IL-17 level (rs=-0.398, P < 0.05). Conclusions Vδ1+/Vδ2+T cell immune imbalance mediated by γδ T cells and over-activation of IL-17 may be involved in the development of HSP, among which the disturbance of immune tolerance induced by Vδ2+T cells plays an important role in the pathophysiology of the disease.
过敏性紫癜 / γ&delta / T细胞 / 细胞凋亡 / IL-17 / 儿童
Henoch-Schönlein purpura / Gamma-delta T cell / Apoptosis / Interleukin-17 / Child
[1] Lei WT, Tsai PL, Chu SH, et al. Incidence and risk factors for recurrent Henoch-Schönlein purpura in children from a 16-year nationwide database[J]. Pediatr Rheumatol Online J, 2018, 16(1):25.
[2] 中华医学会儿科学分会免疫学组,《中华儿科杂志》编辑委员会.儿童过敏性紫癜循证诊治建议[J].中华儿科杂志, 2013, 51(7):502-507.
[3] Brenner MB, McLean J, Dialynas DP, et al. Identification of a putative second T-cell receptor[J]. Nature, 1986, 322(6075):145-149.
[4] Latha TS, Reddy MC, Durbaka PV, et al. γδ T cell-mediated immune responses in disease and therapy[J]. Front Immunol, 2014, 5:571.
[5] Mo WX, Yin SS, Chen H, et al. Amino-bisphosphonates, γδ T cells, and their roles in rheumatoid arthritis[J]. Ann Rheum Dis, 2018, 77(9):e58.
[6] Wu YL, Ding YP, Tanaka Y, et al. γδ T cells and their potential for immunotherapy[J]. Int J Biol Sci, 2014, 10(2):119-135.
[7] 王烨,梁庆红,张莹,等. CD4+T淋巴细胞亚群在儿童过敏性紫癜病理机制中的调控作用[J].中华实用儿科临床杂志, 2015, 30(21):1614-1618.
[8] Fay NS, Larson EC, Jameson JM. Chronic inflammation and γδ T cells[J]. Front Immunol, 2016, 7:210.
[9] de Bruin RCG, Veluchamy JP, Lougheed SM, et al. A bispecific nanobody approach to leverage the potent and widely applicable tumor cytolytic capacity of Vγ9Vδ2-T cells[J]. Oncoimmunology, 2017, 7(1):e1375641.
[10] Wistuba-Hamprecht K, Martens A, Haehnel K, et al. Proportions of blood-borne Vδ1+and Vδ2+T-cells are associated with overall survival of melanoma patients treated with ipilimumab[J]. Eur J Cancer, 2016, 64:116-126.
[11] Ma H, Yuan Y, Zhao L, et al. Association of γδ T cell compartment size to disease activity and response to therapy in SLE[J]. PLoS One, 2016, 11(6):e0157772.
[12] Tham M, Schlör GR, Yerly D, et al. Reduced pro-inflammatory profile of γδ T cells in pregnant patients with rheumatoid arthritis[J]. Arthritis Res Ther, 2016, 18:26.
[13] Edelblum KL, Singh G, Odenwald MA, et al. γδ intraepithelial lymphocyte migration limits transepithelial pathogen invasion and systemic disease in mice[J]. Gastroenterology, 2015, 148(7):1417-1426.
[14] Lo Presti E, Pizzolato G, Gulotta E, et al. Current advances in γδ T cell-based tumor immunotherapy[J]. Front Immunol, 2017, 8:1401.
[15] Pillebout E, Jamin A, Ayari H, et al. Biomarkers of IgA vasculitis nephritis in children[J]. PLoS One, 2017, 12(11):e0188718.
[16] Wang K, Sun X, Cao Y, et al. Risk factors for renal involvement and severe kidney disease in 2731 Chinese children with Henoch-Schönlein purpura:a retrospective study[J]. Medicine (Baltimore), 2018, 97(38):e12520.
[17] Fujii T, Okada M, Craft J. Regulation of T cell-dependent autoantibody production by a γδ T cell line derived from lupusprone mice[J]. Cell Immunol, 2002, 217(1-2):23-35.
[18] Salim M, Knowles TJ, Baker AT, et al. BTN3A1 discriminates γδ T cell phosphoantigens from nonantigenic small molecules via a conformational sensor in its B30.2 domain[J]. ACS Chem Biol, 2017, 12(10):2631-2643.
[19] Robak E, Niewiadomska H, Robak T, et al. Lymphocytes Tγδ in clinically normal skin and peripheral blood of patients with systemic lupus erythematosus and their correlation with disease activity[J]. Mediators Inflamm, 2001, 10(4):179-189.
[20] Mo WX, Yin SS, Chen H, et al. Chemotaxis of Vδ2 T cells to the joints contributes to the pathogenesis of rheumatoid arthritis[J]. Ann Rheum Dis, 2017, 76(12):2075-2084.
[21] Cairo C, Arabito E, Landi F, et al. Analysis of circulating γδ+T cells in children affected by IgE-associated and non-IgEassociated allergic atopic eczema/dermatitis syndrome[J]. Clin Exp Immunol, 2005, 141(1):116-121.
[22] Yin S, Mao Y, Li X, et al. Hyperactivation and in situ recruitment of inflammatory Vδ2 T cells contributes to disease pathogenesis in systemic lupus erythematosus[J]. Sci Rep, 2015, 5:14432.
[23] Jiang X, Park CO, Geddes Sweeney J, et al. Dermal γδ T cells do not freely re-circulate out of skin and produce IL-17 to promote neutrophil infiltration during primary contact hypersensitivity[J]. PLoS One, 2017, 12(1):e0169397.
宁夏医科大学校级项目(XM2018154)。