 PDF(1372 KB)
PDF(1372 KB)


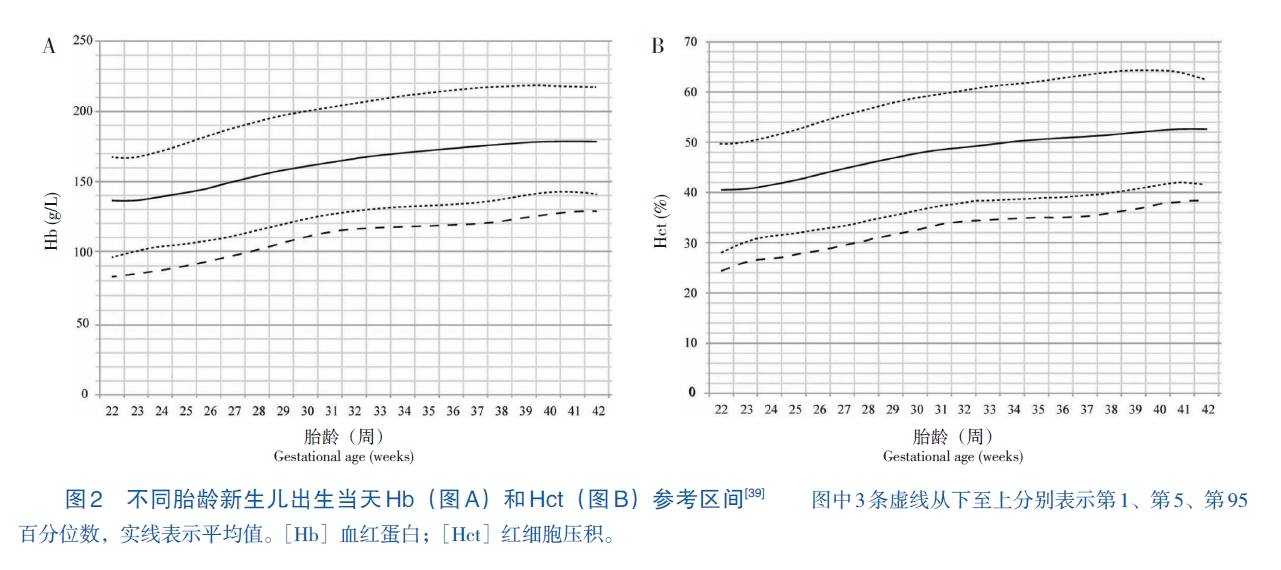
早产儿贫血诊断与治疗的临床实践指南(2025年)
海峡两岸医药卫生交流协会新生儿临床实践指南专家委员会;海峡两岸医药卫生交流协会 新生儿学专业委员会新生儿循证医学学组;《中国当代儿科杂志》编辑部
中国当代儿科杂志 ›› 2025, Vol. 27 ›› Issue (1) : 1-17.
 PDF(1372 KB)
PDF(1372 KB)
 PDF(1372 KB)
PDF(1372 KB)
早产儿贫血诊断与治疗的临床实践指南(2025年)
Clinical practice guidelines for the diagnosis and treatment of anemia of prematurity (2025)
Anemia / Clinical practice guideline / Diagnosis / Treatment / Premature infant