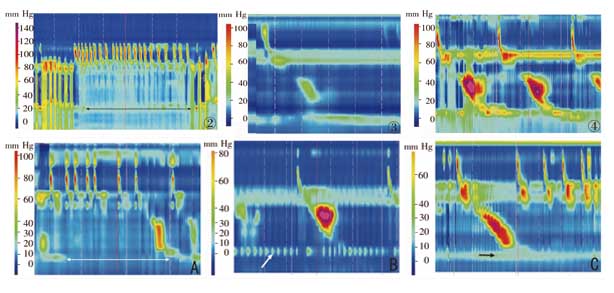
目的:应用食管高分辨测压(HRM)对新生儿食管功能进行检测,为研究新生儿食管功能提供初步依据。方法:应用具有间隔0.75 cm的36个圆周传感器的固态压力测量系统进行新生儿食管HRM,应用ManoView软件对食管蠕动形式进行分析。结果:为11例新生儿成功测压,共记录完整食管蠕动126次。部分受试者可记录到较完全的食管蠕动增压过程,但多数新生儿食管运动模式有别于成人、有其自身的特点。其中可见到吞咽过程中咽部肌肉收缩同时无上食管括约肌(UES)的相应松弛;有多次无效吞咽不伴有食管的蠕动;食管蠕动压力较低;有的足月儿UES 及下食管括约肌(LES)压力较低,但有的早产儿UES 及LES 压力却较高;甚至有的受试者可记录到吞咽后食管全段纵向收缩、LES 上移。结论:新生儿可以安全地进行食管HRM,且耐受性良好。HRM显示新生儿吞咽后可能并不引起食管蠕动,或引起食管的不完全蠕动。新生儿食管功能发育不成熟,个体差异很大,还需大样本的临床数据进一步分析和研究其食管功能的正常及异常情况。
Abstract
OBJECTIVE: To examine the esophageal function of neonates by high resolution manometry (HRM), and to provide preliminary data for research on the esophageal function of neonates. METHODS: Esophageal HRM was performed on neonates using a solid-state pressure measurement system with 36 circumference sensors arranged at intervals of 0.75 cm, and ManoView software was used to analyze esophageal peristalsis pattern. RESULTS: Esophageal HRM was performed successfully in 11 neonates, and 126 occurrences of complete esophageal peristalsis were recorded. Complete esophageal peristalsis with pressure increase was recorded in some neonates but most neonates showed a different esophageal peristalsis pattern compared with adults. Some neonates had no relaxation of the upper esophageal sphincter (UES) when pharyngeal muscles contracted in swallowing, some neonates had multiple swallowing without esophageal peristalsis and some neonates had relatively low pressure of esophageal peristalsis. Full-term infants could have relatively low UES pressure and esophageal sphincter (LES) pressure but some preterm infants showed relatively high UES pressure and LES pressure. Longitudinal contraction of the whole esophagus and elevation of LES after swallowing were recorded in some neonates. CONCLUSIONS: Esophageal HRM is safe and tolerable for neonates. HRM shows that esophageal peristalsis after swallowing may not occur or may be incomplete in neonates. The esophageal function of neonates has not yet been developed completely, with large individual differences in esophageal peristalsis. Large sample data are needed for further analysis and research on the esophageal function of neonates.
关键词
高分辨测压 /
食管 /
新生儿
Key words
High resolution manometry /
Esphogus /
Neonate
{{custom_sec.title}}
{{custom_sec.title}}
{{custom_sec.content}}
参考文献
[1]Fox MR, Bredenoord AJ. Oesophageal high-resolution manometry: moving from research into clinical practice[J]. Gut, 2008, 57(3): 405-423.
[2]Sifrim D, Blondeau K, Mantillla L. Utility of non-endoscopic investigations in the practical management of oesophageal disorders[J]. Best Pract ResClin Gastroenterol, 2009, 23(3): 369-386.
[3]Pandolfino JE, Shi G, Zhang Q, Ghosh S, Brasseur JG, Kahrilas PJ. Measuring EGJ opening patterns using high resolution intraluminal impedance[J]. Neurogastroenterol Motil, 2005, 17(2): 200-206.
[4]Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying esophageal peristalsis with high-resolution manometry: a study of 75asymptomatic volunteers[J]. Am J Physiol Gastrointest Liver Physiol, 2006, 290(5): G988-G997.
[5]Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Kahrilas PJ. Deglutitive upper esophageal sphincter relaxation: a study of 75 volunteer subjects usingsolid-state high-resolution manometry[J]. Am J Physiol Gastrointest Liver Physiol, 2006, 291(3): G525-G531.
[6]Bredenoord AJ, Smout AJ. High-resolution manometry[J]. Dig Liver Dis, 2008, 40(3): 174-181.
[7]Wiesel PH, Maerten P, Guyot J. Investigations for esophageal motility and reflux[J]. Rev Med Suisse, 2009, 5(187): 176-178, 80-84.
[8]Sorin R, Somers S, Austin W, Bester S. The influence of videofluoroscopy on the management of the dysphagic patient[J]. Dysphagia, 1988, 2(3): 127-135.
[9]Palmer JB. Electromyography of the muscles of oropharyngeal swallowing: basic concepts[J]. Dysphagia, 1989, 3(4): 192-198.
[10]Jadcherla SR, Duong HQ, Hofmann C, Hoffmann R, Shaker R. Characteristics of upper oesophageal sphincter and oesophageal body during maturation inhealthy human neonates compared with adults[J]. Neurogastroenterol Motil, 2005, 17(5): 663-670.
[11]Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. Classifying esophageal motility by pressure topography characteristics: a studyof 400 patients and 75 controls[J]. Am J Gastroenterol, 2008, 103(1): 27-37.
[12]Pandolfino JE, Fox MR, Bredenoord AJ, Kahrilas PJ. High-resolution manometry in clinical practice: utilizing pressure topography to classifyoesophageal motility abnormalities[J]. Neurogastroenterol Motil, 2009, 21(8), 796-806.
[13]Dent J. Pathogenesis of gastro-oesophageal reflux disease and novel options for its therapy[J]. Neurogastroenterol Motil, 2008, 20(Suppl 1): 91-102.
[14]Dent J. Approaches to driving the evolving understanding of lower oesophageal sphincter mechanical function[J]. J Smooth Muscle Res, 2007, 43(1): 1-14.
 PDF(1422 KB)
PDF(1422 KB)


 PDF(1422 KB)
PDF(1422 KB)
 PDF(1422 KB)
PDF(1422 KB)