 PDF(1107 KB)
PDF(1107 KB)


潮气呼吸肺功能检测在1~4岁儿童喘息性疾病中的临床应用
韩文, 谢勇, 任淑颖, 尹丽明, 冯晓英, 邓小红, 海新霞
中国当代儿科杂志 ›› 2014, Vol. 16 ›› Issue (8) : 800-804.
 PDF(1107 KB)
PDF(1107 KB)
 PDF(1107 KB)
PDF(1107 KB)
潮气呼吸肺功能检测在1~4岁儿童喘息性疾病中的临床应用
Clinical application of tidal breathing lung function test in 1-4 years old children with wheezing diseases
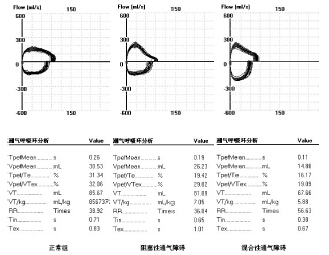
目的 探讨潮气呼吸肺功能检测在1~4 岁儿童喘息性疾病中的临床意义。方法 选择1~4 岁喘息患儿141 例(哮喘41 例、喘息性支气管炎54 例、支气管肺炎46 例)作为观察组,另选取非呼吸道疾病患儿30 例作为对照组,进行潮气呼吸肺功能检测,并观察喘息患儿支气管舒张试验前后肺功能的变化。结果 观察组患儿TBFV 环形态以阻塞性改变为主(65%),达峰时间比(TPTEF/TE)、达峰容积比(VPEF/VE)亦明显低于对照组(P<0.05)。哮喘组支气管舒张试验后TPTEF/TE、VPEF/VE 较试验前明显改善(P<0.05)。以TPTEF/TE、VPEF/VE 任意一个改善率≥ 15% 作为支气管舒张试验的阳性标准,潮气呼吸支气管舒张试验诊断哮喘的灵敏度为47%,特异度为84%。哮喘组患儿舒张试验前TPTEF/TE ≥ 23% 者的阳性率28%,TPTEF/TE<23% 者的阳性率为65%(P<0.05)。结论 1~4 岁喘息患儿肺功能损害以阻塞性通气障碍为主;潮气呼吸支气管舒张试验可在一定程度上反映哮喘气道可逆性特征;在1~4 岁儿童中以潮气呼吸支气管舒张试验诊断哮喘的敏感性不高,但在阻塞程度重的患儿中诊断意义相对较大。
Objective To study the clinical significance of tidal breathing lung function test in 1-4 years old children with wheezing diseases. Methods A total of 141 1-4 years old children with wheezing diseases were enrolled as the observed groups (41 cases of asthma, 54 cases of asthmatic bronchitis, and 46 cases of bronchopneumonia). Thirty children without respiratory diseases were enrolled as the control group. All the recruits underwent tidal breathing lung function test. The observed groups underwent bronchial dilation test, and tidal breathing flow volume (TBFV) parameters were evaluated before and after bronchial dilation test. Results The observed groups showed obstructive ventilatory disorder (65%) according to the TBFV loop, and their ratio of time to peak tidal expiratory flow (TPTEF) to total expiratory time (TE) and ratio of volume to peak expiratory flow (VPEF) to total expiratory volume (VE) were significantly lower than in the control group (P<0.05). The asthma subgroup had significantly improved TPTEF/TE and VPEF/VE after bronchial dilation test (P<0.05). Taking an improvement rate of ≥15% either for TPTEF/TE or for VPEF/VE as an indicator of positive bronchial dilation test, the bronchial dilation test had a sensitivity of 47% and a specificity of 84% in diagnosing asthma in 1-4 years old children. The positive rate was 28% among the children in the asthma subgroup with an TPTEF/TE ratio of ≥23% before bronchial dilation test, versus 65% in those with an TPTEF/TE ratio of <23%. Conclusions Obstructive ventilatory disorder is the main impairment of tidal breathing lung function in 1-4 years old children with wheezing diseases. Tidal breathing bronchial dilation test can reflect a reversal of airway obstruction to a certain extent. The sensitivity of bronchial dilation test for the diagnosis of asthma is not satisfactory in 1-4 years old children with wheezing diseases, but this test has a relatively high diagnostic value in children with severe airway obstruction.
潮气呼吸肺功能 / 支气管肺炎 / 哮喘 / 喘息性支气管炎 / 儿童
Tidal breathing lung function test / Bronchopneumonia / Asthma / Aasthmatic bronchitis / Child