 PDF(2057 KB)
PDF(2057 KB)


 PDF(2057 KB)
PDF(2057 KB)
 PDF(2057 KB)
PDF(2057 KB)
新生儿缺氧缺血性脑病磁共振诊断与损伤类型的分类建议
Patterns of brain injury in neonatal hypoxic-ischemic encephalopathy on magnetic resonance imaging:recommendations on classification
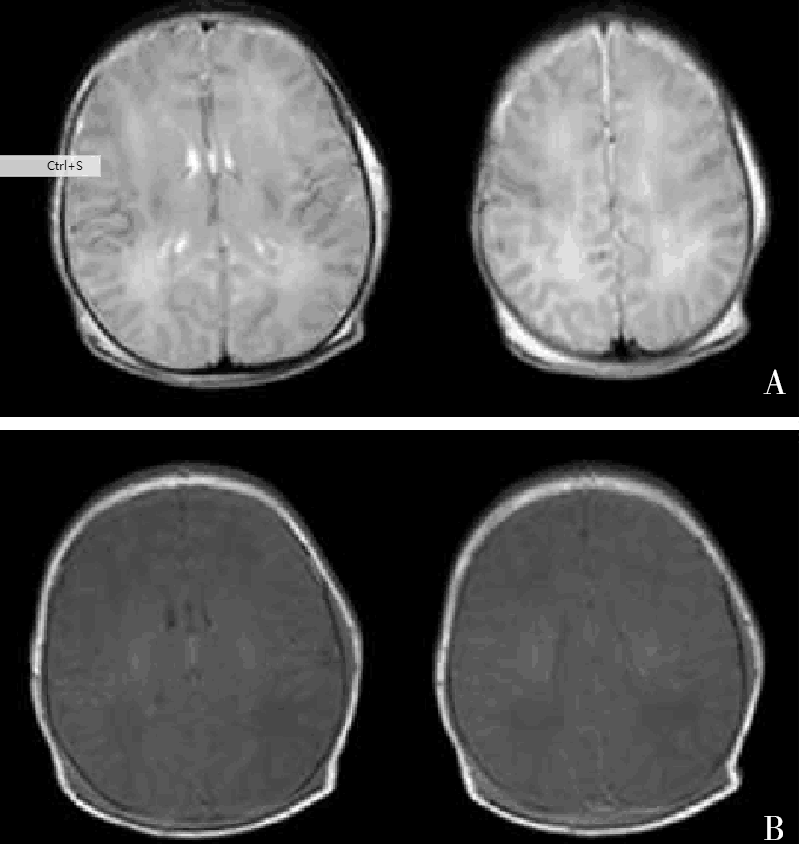
新生儿缺氧缺血性脑病(HIE)有比较统一的临床诊断与分度标准,但是符合相同诊断标准的窒息所致HIE的临床表现、神经病理损伤类型有很大差异。磁共振成像(MRI)能很好地呈现HIE损伤类型、损伤进程,且与其远期神经发育结局密切相关,但不同MRI检查序列所反映的损伤表现可能不尽相同。弥散加权序列适宜的检查时间为出生后2~4 d,常规序列为出生后的4~8 d。HIE的MRI主要损伤类型有丘脑基底节+内囊后肢损伤、分水岭样损伤累及皮层和皮层下白质、局灶-多灶性微小性白质损伤,以及广泛全脑性损伤。严重的急性产时窒息易导致深部灰质损伤(丘脑基底节),也可累及脑干,锥体束是最易受累的白质纤维束,而反复间断性缺氧缺血以及伴有感染、低血糖等易导致分水岭区和深部白质损伤。但上述损伤类型有时很难明确区分,而是以某一类型为主,并非所有HIE都有特征性的MRI表现。
Although there are unified criteria for the clinical diagnosis and grading of neonatal hypoxic-ischemic encephalopathy (HIE), clinical features and neuropathological patterns vary considerably among the neonates with HIE due to birth asphyxia in the same classification. The patterns and progression of brain injury in HIE, which is closely associated with long-term neurodevelopment outcomes, can be well shown on magnetic resonance imaging (MRI), but different sequences may lead to different MRI findings at the same time. It is suggested that diffusion-weighted imaging sequence be selected at 2-4 days after birth, and the conventional MRI sequence at 4-8 days. The major patterns of brain injury in HIE on MRI are as follows:injury of the thalamus and basal ganglia and posterior limbs of the internal capsules; watershed injury involving the cortical and subcortical white matter; focal or multifocal minimal white matter injury; extensive whole brain injury. Severe acute birth asphyxia often leads to deep grey matter injury (thalamus and basal ganglia), and the brain stem may also be involved; the pyramidal tract is the most susceptible white matter fiber tract; repetitive or intermittent hypoxic-ischemic insults, with inflammation or hypoglycemia, usually cause injuries in the watershed area and deep white matter. It is worth noting that sometimes the pattern of brain injury among those described above cannot be determined exactly, but rather a predominant one is identified; not all cases of HIE have characteristic MRI findings.
Cerebral hypoxia / Hypoxic-ischemic encephalopathy / Magnetic resonance imaging / Neonate
[1] Robertson NJ, Tan S, Groenendaal F, et al. Which neuroprotective agents are ready for bench to bedside translation in the newborn infant?[J]. J Pediatr, 2012, 160(4):544-552.e4.
[2] Phelan JP, Korst LM, Martin GI. Application of criteria developed by the task force on neonatal encephaloapthy and cerebral palsy to acutely asphyxiated neonates[J]. Obstet Gynecol, 2011, 118(4):824-830.
[3] Graham EM, Ruis KA, Hartman AL, et al. A systematic review of the role of intrapartum hypoxia-ischemia in the causation of neonatal encephaloapthy[J].Am J Obstet Gynecol, 2008, 199(6):587-595.
[4] 中华医学会儿科学分会新生儿学组.新生儿缺氧缺血性脑病诊断标准[J].中国当代儿科杂志, 2005, 7(2):97-98.
[5] Barkovich AJ, Westmark K, Partridge C, et al. Perinatal asphyxia:MR findings in the first 10 days[J]. AJNR Am J Neuroradiol, 1995, 16(3):427-438.
[6] Volpe JJ. Neonatal encephalopathy:an inadequate term for hypoxic-ischemic encephaloapthy[J]. Ann Neurol, 2012, 72(2):156-166.
[7] Barkovich AJ, Miller SP, Bartha A, et al. MR imaging, MR spectroscopy,and diffusion tensor imaging of sequential studies in neonates with encephalopathy[J]. AJNR Am J Neuroradiol, 2006, 27(3):533-547.
[8] Thayyil S, Chandrasekaran M, Taylor A, et al. Cerebral magnetic resonance biomarkers in neonatal encephalopahty:a meta-analysis[J]. Pediatrics, 2010, 125(2):e382-e395.
[9] Rutherford M, Ramenghi LA, Edwarsds AD, et al. Assessment of brain tissue injury after moderate hypothermia in neonates with hypoxic-ischemic encephaloapthy:a nested substudy of a randomized controlled trial[J]. Lancet Neurol, 2010, 9(1):39-45.
[10] Cheong JL, Coleman L, Hunt RW, et al. Prognostic utility of magnetic resonance imaging in neonatal hypoxic-ischemic encephalopahty[J]. Arch Pediatr Adolesc Med, 2012, 166(7):634-640.
[11] Rutherford M, Malamatensiou C, McGuinness A, et al. Magnetic resonance imaging in hypoxic-ischemic encephalopathy[J]. Early Hum Dev, 2010, 86(3):351-360.
[12] Holshouser BA, Ashwal S, Shu S, et al. Proton MR spectroscopy in children with acute brain injury:comparison of short and long echo time acquisitions[J]. J Magn Reson Imaging, 2000, 11(1):9-19.
[13] Roelants-Van Rijn AM, van der Grond J, de Vries LS, et al. Value of 1H-MRS using different echo times in neonates with cerebral hypoxia-ischemia[J]. Pediatr Res, 2001, 49(3):356-362.
[14] Azzopardi D, Edwards AD. Magnetic resonance biomarkers of neuroprotective effects in infants with hypoxic-ischemi encephaloapthy[J]. Semin Fetal Neonatal Med, 2010, 15(2):261-269.
[15] McKinstry RC, Miller JH, Snyder AZ, et al. A prospective, longitudinal diffusion tensor imaging study of brain injury in newborns[J]. Neurology, 2002, 59(6):824-833.
[16] Bednarek N, Mathur A, Inder T, et al. Impact of therapeutic hypothermia on MRI diffusion changes in neonatal encephalopathy[J]. Neurology, 2012, 78(18):1420-1427.
[17] Ment LR, Bada HS, Barnes P, et al. Practice parameter:Neuroimaging of the neonate:report of the quality standards subcommittee of the American academy of neurology and the practice committee of the child neurology society[J]. Neurology, 2002, 58(12):1726-1738.
[18] Barkovich AJ, Hajnal BL, Vigneron D, et al. Prediction of neuromotor outcome in perinatal asphyxia:evaluation of MR scoring systems[J]. AJNR Am J Neuroradiol, 1998, 19(1):143-149.
[19] Perlman JM. Intrapartum asphyxia and cerebral palsy is there link?[J]. Clin Perinatol, 2006, 33(2):335-353.
[20] Otaduy MC, Leite CC, Lacerda MT, et al. Proton MR spectroscopy and imaging of a galactosemic patient before and after dietary treatment[J]. AJNR Am J Neuroradiol, 2006, 27(1):204-207.
[21] Chau V, Poskitt KJ, Sargent MA, et al.Comparison of computer tomography and magnetic resonance imaging scans on the third day of life in term newborns with neonatal encephalopathy[J]. Pediatrs, 2009, 123(1):319-326.
[22] Martinez-Biarge M, Bregant T, Countney J, et al. White matter and cortical injury in hypoxic-ischemic encephalopathy:antecedent factor and 2 year outcome[J]. J Pediatr, 2012, 161(5):799-807.
[23] Li AM, Chau V, Poskitt KJ, et al. White matter injury in term newborns with neonatal encephalopathy[J]. Pediatr Res, 2009, 65(1):85-89.
[24] Barrett MJ, Donoghue V, Mooney EE, et al. Isolated acute non-cystic white matter injury in term infants presenting with neonatal encephalopathy[J]. Arch Dis Child Fetal Neonatal, 2013, 98(2):F158-F160.
[25] Harteman JC, Nikkels PG, Benders MJ, et al. Placental pathology in full-term infants with hypoxic-ischemic neonatal encephalopathy and association with magnetic resonance imaging pattern of brain injury[J]. J Pediatr, 2013, 163(4):968-995.e2.
[26] Martinez-Biarge M, Diez-Sebastian J, Rurherford MA, et al. Outcome after central grey matter injury in term perinatal hypoxic-ischemic encephalopathy[J]. Early Hum Dev, 2010, 86(11):675-682.
[27] Martinez-Biarge M, Diez-Sebastian J, Kapellou O, et al. Predicting motor outcome and death in term hypoxic-ischemic encephalopathy[J]. Neurology, 2011, 76(24):2055-2061.
[28] Wong DS, Poskitt KJ, Chau V, et al. Brai injury patterns in hypoglycemia in neonatal encephalopathy[J]. AJNR Am J Neuroradiol, 2013, 34(7):1456-1461.